How Is IVF Done? Your Step-by-Step Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is like a helping hand for people dreaming of starting a family but facing roadblocks along the way. It’s a process that blends science, hope, and a little bit of patience to make parenthood possible. Maybe you’ve heard about it from a friend, seen it in the news, or stumbled across stories on social media—IVF is everywhere these days, and for good reason. It’s helped millions of people welcome babies into their lives, with over 10 million little ones born worldwide thanks to this technology. But how does it actually work? Let’s walk through it together, step by step, in a way that feels like chatting with a friend over coffee.
IVF isn’t just one quick procedure—it’s a journey with several stages, each one carefully designed to boost the chances of success. Whether you’re curious about the process, considering it for yourself, or just want to understand what a loved one might be going through, this guide has you covered. We’ll break it down into bite-sized pieces, sprinkle in some real-world insights, and even share a few things you won’t find in most articles—like what the latest research says about improving outcomes or how small lifestyle tweaks can make a difference.
What Is IVF, Anyway?
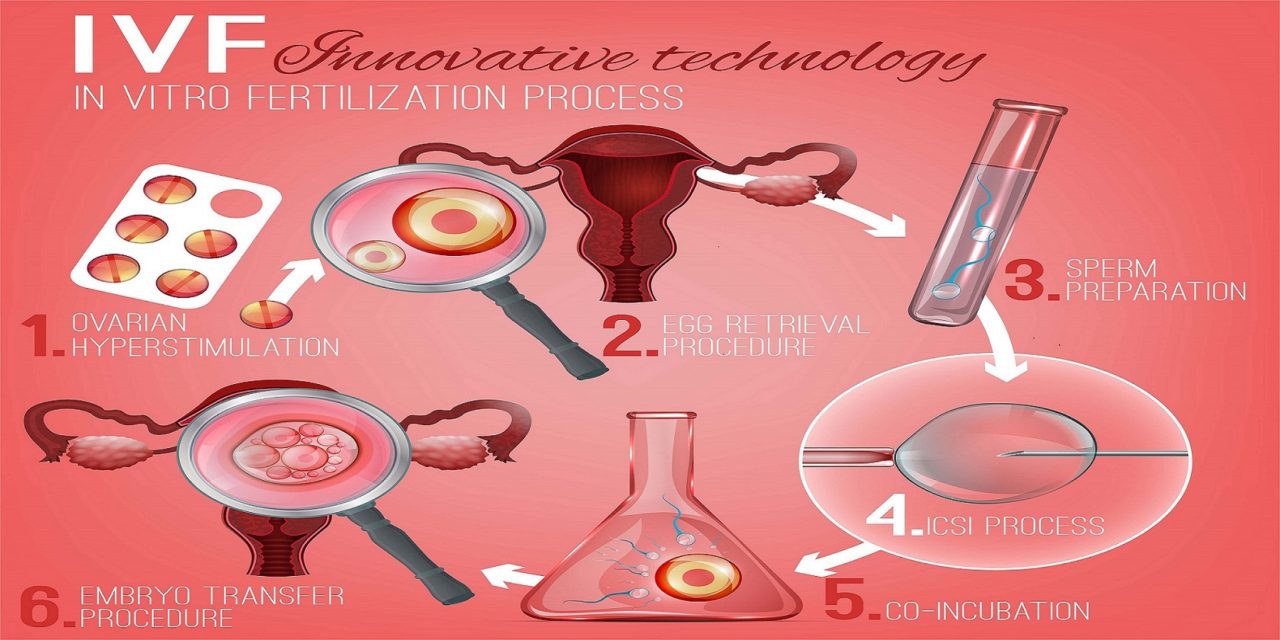
IVF stands for “in vitro fertilization,” which is a fancy way of saying “fertilization in a glass.” The “in vitro” part comes from Latin, meaning it happens outside the body—in a lab, to be exact. Picture this: instead of an egg and sperm meeting naturally inside a person’s body, doctors bring them together in a petri dish. Once they form an embryo (a fertilized egg), it’s placed back into the uterus to grow into a baby. Simple in theory, right? But there’s a lot going on behind the scenes to make it happen.
This process is part of a bigger family of treatments called assisted reproductive technology (ART). It’s often a go-to for people dealing with infertility—things like blocked fallopian tubes, low sperm counts, or unexplained struggles to conceive. But it’s not just for infertility anymore. Some use IVF to avoid passing on genetic conditions, while others, like same-sex couples or single parents, turn to it with the help of donors or surrogates. It’s versatile, and it’s changing lives every day.

Step 1: Getting the Ovaries Ready with Stimulation
The IVF journey kicks off with a boost to the ovaries. Normally, your body releases just one egg each month during ovulation. But in IVF, doctors want more eggs to work with—more eggs mean more chances for a healthy embryo. To make this happen, you’ll take hormone medications for about 9 to 12 days.
These meds usually come as injections (don’t worry, they’re tiny needles!), and they contain hormones like follicle-stimulating hormone (FSH) and luteinizing hormone (LH). Think of them as cheerleaders for your ovaries, encouraging them to grow multiple follicles—those are the little sacs where eggs mature. You’ll visit the clinic a few times during this phase for ultrasounds and blood tests to check how those follicles are coming along.
What’s It Like?
- The Good: Most people handle the shots just fine. You might feel a little bloated or moody—like a mild version of PMS—but it’s temporary.
- The Tricky Part: Some folks experience a rare condition called ovarian hyperstimulation syndrome (OHSS), where the ovaries overreact, causing swelling or discomfort. It’s not common, but your doctor will keep an eye out.
Pro Tip
Start a mini journal to track how you feel each day. It’s a simple way to spot patterns and feel more in control during this whirlwind.
Step 2: Triggering the Eggs to Mature
Once your follicles look ready—usually when they’re about 18-20 millimeters wide—it’s time for the “trigger shot.” This is another injection, often human chorionic gonadotropin (hCG), that tells your eggs, “Hey, it’s time to finish growing!” It mimics the natural hormone surge that happens before ovulation.
Timing is everything here. About 36 hours after the trigger shot, your eggs will be ripe for the picking. Too early or too late, and the eggs might not be ready or could already be gone. That’s why your doctor schedules the next step—the egg retrieval—down to the hour.
Fun Fact
Did you know the trigger shot is so precise that some clinics have patients set alarms to take it at, say, 2 a.m.? It’s like a secret mission for your future baby!
Step 3: Egg Retrieval—Harvesting the Goods
Now comes the big moment: egg retrieval. This is a quick procedure, usually done under light sedation so you’re comfy and snoozing through it. The doctor uses a thin needle guided by ultrasound to gently pull the eggs out of your ovaries through the vaginal wall. It sounds intense, but it only takes about 20-30 minutes.
You’ll wake up feeling a bit groggy, maybe with some mild cramping—like a light period. Most people head home the same day and take it easy with a heating pad and Netflix. On average, doctors retrieve 8-15 eggs, though it varies depending on your age, health, and how your ovaries responded to the meds.
What to Expect
- ✔️ Quick Recovery: Rest for a day, and you’re usually back to normal.
- ❌ Watch Out: Rare risks include bleeding or infection, but they’re super uncommon with today’s tech.
Insider Tip
Bring a cozy blanket to the clinic. It’s a small comfort that makes the sterile room feel more like home.

Step 4: Sperm Collection and Fertilization
While you’re resting post-retrieval, the other half of the equation comes into play: sperm. If you’re using a partner’s sperm, they’ll provide a sample that day (yep, in a private room at the clinic). If you’re using a donor, that’s already arranged ahead of time.
In the lab, the magic happens. There are two main ways to fertilize the eggs:
- Traditional IVF: Sperm and eggs are mixed in a dish, and nature takes its course—about 65-80% of eggs fertilize this way.
- ICSI (Intracytoplasmic Sperm Injection): A single sperm is injected directly into an egg. This is a game-changer for low sperm counts or motility issues, and it’s becoming more common, with some clinics using it in nearly every case.
Why It Matters
ICSI has bumped up success rates big time. A 2023 study from the American Society for Reproductive Medicine found that ICSI pregnancies rose by 15% over the past decade, especially for tricky cases.
Step 5: Growing Embryos in the Lab
Once fertilized, the eggs become embryos and move into a special incubator. For the next 2-5 days, embryologists watch them grow, checking for healthy cell division. By day 5, the best embryos reach the blastocyst stage—think of it as the “ready-to-plant” phase.
Not all embryos make it this far, and that’s normal. Some stop growing early, which is why starting with more eggs helps. If you’re doing genetic testing (like preimplantation genetic diagnosis, or PGD), this is when they’d take a tiny sample from each embryo to screen for conditions like cystic fibrosis.
Interactive Quiz: How Many Embryos Survive?
How many eggs do you think turn into blastocysts on average?
- A) 90%
- B) 50-60%
- C) 20%
(Answer: B! About half make it, but it depends on age and egg quality.)
Step 6: Embryo Transfer—Planting the Seed
Time to put those embryos to work! The transfer is a simple procedure—no sedation needed. The doctor threads a thin catheter through your cervix and places one or two embryos into your uterus. You’ll see it all on an ultrasound screen, which is pretty cool—like watching your future unfold in real-time.
Afterward, you’ll lie down for a bit, then head home. Some clinics suggest taking it easy for a day or two, but there’s no hard rule to stay in bed. In fact, a 2024 study in Fertility and Sterility found no difference in success rates between resting and resuming light activity.
Fresh vs. Frozen
- Fresh Transfer: Done right after retrieval, in the same cycle.
- Frozen Transfer: Embryos are frozen and transferred later. This is trending up because it lowers OHSS risk and lets your body recover first.
Step 7: The Two-Week Wait and Pregnancy Test
Now, the hardest part: waiting. About 10-14 days after the transfer, you’ll take a blood test to see if you’re pregnant. This “two-week wait” can feel endless, with every twinge making you wonder, “Is it working?”
Coping Tips
- ✔️ Try light walks or yoga to ease stress.
- ❌ Avoid Googling every symptom—it’s a rabbit hole!
If the test is positive, congrats—you’re on your way! If not, don’t lose hope. Many people need a few cycles, and your doctor can tweak the plan.
What Makes IVF Success Tick?
Success isn’t guaranteed, and that’s the tough truth. Your odds depend on a few big factors:
- Age: Under 35? You’ve got a 40-50% chance per cycle. Over 40? It drops to 10-20%.
- Egg Quality: Younger eggs tend to work better, which is why donor eggs can boost success for older patients.
- Clinic Expertise: Top clinics with cutting-edge labs see higher rates.
A 2025 report from the CDC showed live birth rates climbed 8% since 2020, thanks to better freezing tech and personalized protocols. But it’s not one-size-fits-all—your story is unique.
Beyond the Basics: What You Might Not Know
Most articles stop at the steps, but there’s more to the IVF picture. Here are three things you won’t find everywhere:
1. The Power of Mild IVF
Ever heard of mild stimulation IVF? It uses lower doses of meds or skips them entirely (natural cycle IVF). It’s gentler on your body and wallet, though success rates dip a bit—around 20-30% per cycle vs. 40-50% with standard IVF. A 2024 study in Human Reproduction found it’s gaining traction for women with medical conditions or those who want a less intense option.
2. Lifestyle Tweaks That Help
Sure, you’ve heard “eat healthy,” but did you know caffeine might mess with your odds? A 2023 study from the University of California linked high caffeine intake (over 200 mg daily—about two coffees) to a 10% drop in IVF success. Swap in herbal tea and watch your sleep, too—7-8 hours a night can balance hormones.
3. The Emotional Rollercoaster
IVF isn’t just physical—it’s a mental marathon. A 2025 survey by Resolve: The National Infertility Association found 70% of patients felt “overwhelmed” during treatment. Yet only 30% sought support. Joining a group or chatting with a counselor can lighten the load—think of it as a lifeline, not a luxury.
Real Stories: IVF in Action
Meet Sarah, a 34-year-old teacher from Ohio. After two years of trying naturally, she and her husband turned to IVF. “The shots were the worst part,” she says, “but seeing those embryos on the screen? Pure magic.” Their first cycle worked, and their son just turned one. Then there’s James, 42, who used ICSI after a low sperm count diagnosis. It took three rounds, but he’s now dad to twins. These stories show IVF’s highs and lows—and its power to rewrite endings.
What’s New in IVF? The Latest Buzz
IVF isn’t standing still. Here’s what’s hot in 2025:
- AI in Embryo Selection: Clinics are using artificial intelligence to pick the best embryos, boosting success by up to 15%, per a Nature Medicine study.
- Lab-on-a-Chip Tech: Tiny devices might soon automate parts of IVF, cutting costs and human error. It’s still experimental, but the future’s bright.
- Fertility Preservation Boom: More young people are freezing eggs or embryos early, driven by career goals or health concerns. X posts show this trend spiking, with #EggFreezing up 25% this year.
Poll Time!
What excites you most about IVF’s future?
- A) Cheaper treatments
- B) Higher success rates
- C) Easier process
(Share your pick in the comments!)
Your IVF Toolkit: Practical Advice
Ready to dive in? Here’s how to prep like a pro:
- Ask Questions: Grill your clinic about their success rates, protocols, and costs—transparency is key.
- Build a Support Squad: Tell a friend or family member what you need, whether it’s a ride or a vent session.
- Mind Your Body: Cut back on alcohol and stress—studies show even one drink a day can lower odds by 5%.
Checklist for Day 1
- ✔️ Comfy clothes for appointments
- ✔️ A water bottle (hydration helps!)
- ❌ No heavy lifting post-retrieval
Wrapping It Up: IVF Is a Journey Worth Exploring
IVF is more than a medical process—it’s a path to possibility. From the first shot to that final test, every step is a mix of science and heart. It’s not always easy, and it’s not always fast, but for so many, it’s the bridge to a dream come true. Whether you’re just curious or ready to take the plunge, knowing how it works puts you in the driver’s seat.
Got questions? Drop them below—I’d love to hear what’s on your mind. And if you’ve been through IVF, share your story. You never know who it might inspire.




