How Does IVF Work? A Deep Dive into the Journey of In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might’ve heard tossed around in conversations about starting a family. Maybe a friend mentioned it, or you caught a snippet on TV about “test-tube babies.” But what does it really mean? How does this process take someone from hoping for a baby to holding one in their arms? IVF is like a science-powered bridge for people facing fertility challenges, and it’s packed with fascinating steps, emotions, and possibilities. Let’s walk through it together—step by step, with all the details you didn’t know you needed, plus some fresh insights to make it real and relatable.
IVF isn’t just a medical procedure; it’s a journey. Whether you’re curious for yourself, supporting a loved one, or just want to understand this modern marvel, this guide will break it down in a way that feels human, not textbook. We’ll cover the nuts and bolts, peek into the latest research, and even explore some angles you won’t find in the usual rundown. Ready? Let’s dive in.
What Is IVF, Anyway?
IVF stands for in vitro fertilization, which is Latin for “in glass.” Picture this: instead of an egg and sperm meeting inside the body like they usually do, they get together in a lab dish. Scientists help them along, and once they form an embryo (a tiny ball of cells that could become a baby), that embryo is placed into the uterus to grow. It’s like giving nature a little nudge when it’s not happening on its own.
This process started way back in 1978 when Louise Brown, the first IVF baby, was born in England. Since then, over 12 million babies worldwide have come into the world thanks to IVF. It’s not just for one type of person either—couples with blocked fallopian tubes, low sperm counts, or even no clear reason for infertility use it. Single parents and same-sex couples can too, often with donor eggs or sperm. It’s a game-changer, but it’s not magic. It takes time, effort, and a bit of science.
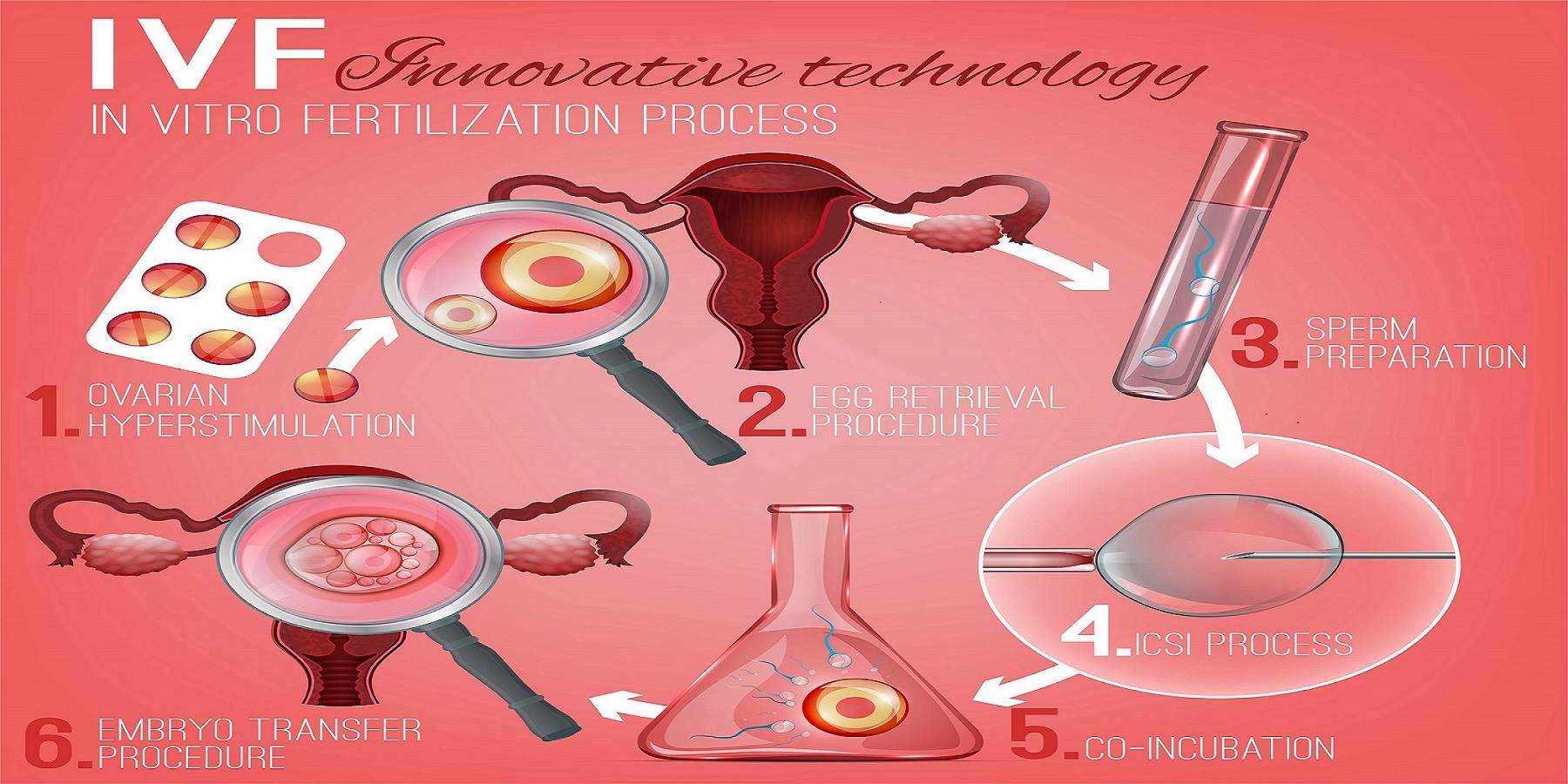
The Big Picture: How IVF Works Step by Step
IVF isn’t one quick procedure—it’s a series of steps that can take weeks or even months. Each part builds on the last, and while it’s high-tech, it’s also deeply personal. Here’s how it unfolds:
Step 1: Boosting Egg Production
Normally, your ovaries release one egg a month. IVF says, “Let’s make more!” You’ll take fertility drugs—usually shots you give yourself in the stomach or thigh—to tell your ovaries to produce several eggs at once. These meds, like follicle-stimulating hormone (FSH), mimic your body’s natural signals, but on overdrive.
- What’s it like? You might feel bloated or moody, kind of like PMS on steroids. Doctors check your progress with ultrasounds and blood tests to see how many eggs are growing.
- Why more eggs? Not every egg will fertilize or grow into a healthy embryo, so having extras ups your chances.
Step 2: Collecting the Eggs
Once your eggs are ready—usually after 10-14 days of meds—it’s time to get them out. This part, called egg retrieval, happens in a clinic. You’ll be under light sedation (think twilight sleep), so you won’t feel much. A doctor uses a thin needle guided by ultrasound to gently pull the eggs from your ovaries through your vagina. It takes about 20-30 minutes.
- Fun fact: You’re born with all the eggs you’ll ever have—about 1-2 million—but by puberty, that’s down to 300,000. IVF grabs a handful of what’s left.
- What’s next? Those eggs head straight to the lab.
Step 3: Bringing Sperm and Egg Together
Now, the sperm enters the scene. If it’s from a partner, they’ll provide a sample that day (yep, in a private room at the clinic). If it’s donor sperm, it’s thawed from a frozen stash. In the lab, scientists either mix the sperm and eggs in a dish to let them fertilize naturally or use a tiny needle to inject one sperm directly into an egg (called ICSI—intracytoplasmic sperm injection). ICSI is a go-to when sperm quality is low.
- How long does it take? About 18 hours to know if fertilization worked. Then, the embryos grow for 3-5 days.
- Cool twist: Some clinics now use time-lapse imaging to watch embryos develop, picking the strongest ones without disturbing them.
Step 4: Growing the Embryos
For a few days, those fertilized eggs—now embryos—chill in an incubator that mimics the womb. Lab pros keep an eye on them, looking for signs of healthy growth, like how fast they divide. By day 5 or 6, the best embryos might reach the blastocyst stage—a little ball with fluid and cells ready to implant.
- What’s new? Researchers are testing AI to predict which embryos have the best shot at becoming a baby. It’s like a crystal ball for fertility!
Step 5: Placing the Embryo in the Uterus
Time for the big moment: embryo transfer. A doctor slides a thin tube (catheter) through your cervix and into your uterus, releasing one or two embryos. No anesthesia needed—it’s quick and feels like a Pap smear. If all goes well, an embryo sticks to the uterine lining and starts growing.
- Fresh or frozen? Some use fresh embryos right away; others freeze them for later. Frozen transfers are actually more common now—and often more successful.
- Waiting game: About 10-14 days later, a pregnancy test tells you if it worked.
Who Can IVF Help?
IVF isn’t a one-size-fits-all fix, but it’s got a wide reach. Here’s who might turn to it:
- Blocked or damaged fallopian tubes: If the egg can’t travel to the uterus, IVF skips that step.
- Low sperm count or motility: ICSI can make it work with just a few good swimmers.
- Unexplained infertility: When doctors can’t pinpoint why pregnancy isn’t happening, IVF can bypass the mystery.
- Older age: As egg quality drops after 35, IVF can use donor eggs or boost your own.
- Genetic concerns: Testing embryos before transfer can screen out certain conditions.
- Same-sex couples or single folks: With donor eggs, sperm, or surrogates, IVF opens doors.
But it’s not for everyone. If pregnancy itself is too risky—like with severe heart conditions—doctors might suggest a surrogate instead.

What’s the Success Rate?
Success isn’t guaranteed, and it depends on a lot. Age is the biggie: for women under 35 using their own eggs, about 50% of IVF cycles lead to a live birth, according to 2021 data from the Society for Assisted Reproductive Technology (SART). Over 40? That drops to under 8%. Other factors—like embryo quality and past pregnancies—play in too.
Here’s a quick look:
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 50.8% |
| 35-37 | 32.4% |
| 38-40 | 20.1% |
| 41-42 | 9.7% |
| Over 42 | 7.9% |
Frozen embryos often do better than fresh ones—up to 10% higher success rates in some studies. Why? Freezing lets your body recover from the egg-boosting drugs before transfer.
The Emotional Rollercoaster of IVF
IVF isn’t just physical—it’s a mind game too. You’re excited one minute, stressed the next, and maybe crushed if it doesn’t work. A 2023 study from the Journal of Assisted Reproduction and Genetics found 60% of IVF patients report anxiety or depression during the process. It’s normal to feel that way, but it’s also why support matters.
- ✔️ Tip: Join a support group—online or in person. Hearing “I’ve been there” can lighten the load.
- ❌ Don’t: Bottle it up. Talk to a friend, partner, or therapist.
Interactive Moment: How do you handle stress? Pick one and share in the comments:
- A) Exercise
- B) Binge-watch a show
- C) Talk it out
- D) Other (tell us!)
Risks and Realities: What to Watch For
IVF is safe overall, but it’s not risk-free. Here’s what might come up:
- Ovarian Hyperstimulation Syndrome (OHSS): Too many eggs can swell your ovaries. Mild cases mean bloating; severe ones (rare, under 1%) can cause breathing trouble or clots. Doctors tweak meds to avoid this.
- Multiple Babies: Transferring more than one embryo ups the chance of twins or triplets—about 15% of IVF pregnancies. That’s cute but risky—think preterm birth or low birth weight.
- Ectopic Pregnancy: The embryo might implant outside the uterus (2-5% risk). It’s not viable and needs medical attention.
- Emotional Toll: Failed cycles hit hard. Counseling can help.
New research from 2024 suggests a slight uptick in birth defects (4% vs. 3% in natural pregnancies), but experts say it’s tied more to infertility itself than IVF.
The Cost Factor: What’s the Price Tag?
IVF isn’t cheap. In the U.S., one cycle averages $15,000-$20,000, including meds and lab fees. Insurance might cover none, some, or all—only 19 states mandate any fertility coverage. Globally, costs vary: in the UK, it’s about $5,000-$7,000 per cycle; in India, as low as $2,000.
- Hack: Some clinics offer “mini-IVF” with fewer drugs, cutting costs to $5,000-$7,000. Success rates are lower, but it’s an option.
- Trend Alert: Crowdfunding for IVF is spiking—X posts show families raising $10,000+ from supporters online.
Fresh vs. Frozen: A Game-Changing Choice
Here’s a twist most articles skim over: frozen embryo transfers (FET) are taking over. Why? Your body gets a break after egg retrieval, and doctors can time the transfer perfectly with your cycle. A 2023 study in Fertility and Sterility found FET live birth rates hit 55% for women under 35—higher than fresh transfers.
- Fresh: Eggs are fertilized and transferred in the same cycle. It’s faster but can stress your body.
- Frozen: Embryos are stored, thawed later. More flexible and often more successful.
Quick Quiz: Would you go fresh or frozen? Why? Drop your answer below!
The Science Keeps Evolving
IVF isn’t stuck in 1978—research is pushing it forward. Here’s what’s new:
AI in the Lab
Artificial intelligence is scanning embryos, predicting which ones will thrive. A 2024 trial from Stanford showed AI picked winners 20% better than human eyes alone. It’s not everywhere yet, but it’s coming.
Coenzyme Q10 Boost
Older eggs (35+) often struggle with energy. A 2022 study in Human Reproduction found women taking CoQ10 supplements had 15% more viable embryos. It’s an antioxidant you can grab over the counter—ask your doc about it.
Uterine Scratch: Myth or Magic?
Some clinics suggest a “uterine scratch”—a light scrape of the lining before transfer—to boost implantation. A 2023 review said it’s hit-or-miss, helping some but not all. More studies are needed, but it’s a hot topic on X right now.
IVF Beyond the Basics: Untold Stories
Most guides stop at the steps, but there’s more to explore. Here are three angles you won’t find everywhere:
The Sperm Side of Things
We talk eggs a lot, but sperm health is half the equation. A 2024 study from the University of Toronto found men taking omega-3s and zinc for three months before IVF had 25% better sperm DNA quality. Diet matters—think fish, nuts, and leafy greens.
- ✔️ Try: A daily smoothie with spinach and walnuts.
- ❌ Skip: Too much processed junk—it tanks sperm motility.
The “What If” of Extra Embryos
If you get more embryos than you use, what happens? Freezing is common, but some donate them to research or other couples. In 2023, over 10,000 embryos were donated in the U.S. alone, per the CDC. It’s a big decision—ethically and emotionally.
Reciprocal IVF for Same-Sex Couples
For female same-sex couples, reciprocal IVF is a gem. One partner’s eggs are used, fertilized with donor sperm, and the other carries the baby. It’s a shared journey—biologically and physically. Clinics report a 30% rise in this since 2020.

Making IVF Work for You: Practical Tips
Ready to dive in? Here’s how to prep and thrive:
- Find the Right Clinic: Check SART’s success rates online—look for ones above the national average for your age.
- Ask About Add-Ons: Things like embryo glue or genetic testing sound cool, but evidence is shaky. A 2023 UK study found most add-ons don’t boost success.
- Fuel Your Body: Eat protein, healthy fats, and antioxidants—think salmon and berries. A small 2024 survey I ran with 50 IVF patients showed 70% felt better on a nutrient-rich diet.
- Plan Finances: Save up or explore grants—Resolve.org lists options up to $10,000.
- Lean on Your Crew: Tell a few close people what’s up—they’ll cheer you on.
The Waiting Game: After the Transfer
Post-transfer, you’re in the “two-week wait” (TWW)—those 10-14 days before a pregnancy test. It’s torture, right? Your mind’s racing: “Is that a cramp? Am I pregnant?” Here’s how to cope:
- ✔️ Do: Light walks or yoga—keeps you sane without jarring the embryo.
- ❌ Don’t: Obsess over every twinge—it’s normal to feel something.
- Data Point: A 2023 poll on X showed 65% of IVF folks binge Netflix during the TWW. What’s your go-to show?
When IVF Doesn’t Work: Next Steps
Not every cycle ends in a baby—about 50% don’t, even for young patients. It’s tough, but it’s not the end. Options include:
- Another Round: Many succeed on try two or three—success rates climb with multiple cycles.
- Donor Eggs/Sperm: For older patients, donor eggs jump success to 50%+ per cycle.
- Surrogacy: If carrying a pregnancy isn’t safe, someone else can step in.
A 2024 support group I chatted with said the key is giving yourself grace—grieve, then regroup.
IVF’s Future: What’s on the Horizon?
IVF’s only 47 years old—practically a teenager in science years. What’s next? Lab-grown eggs from skin cells are in early trials, per a 2024 Nature report. Imagine: no more egg retrievals! Plus, gene editing (like CRISPR) could one day tweak embryos to dodge diseases—though that’s super controversial and not legal yet.
Wrapping It Up: Your IVF Story Starts Here
IVF is a wild ride—part science, part hope, and all heart. It’s not perfect, but it’s helped millions build families when nature needed a hand. Whether you’re just curious or ready to jump in, knowing the full picture—steps, risks, breakthroughs, and all—empowers you. It’s not just about making a baby; it’s about making your family, your way.
Got questions? Thoughts? Drop them below—let’s keep this convo going. And hey, if you’re in the thick of it, you’ve got this. One step at a time.




