How Does IVF Work? A Step-by-Step Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is like a helping hand for people dreaming of starting a family but facing roadblocks along the way. It’s a process that blends science, hope, and a little bit of patience to make parenthood possible for those who might otherwise struggle. If you’ve ever wondered what happens behind the scenes of this life-changing procedure, you’re in the right place. This guide will walk you through every step, sprinkle in some fresh insights, and answer questions you didn’t even know you had—all in a way that feels like chatting with a friend over coffee.
IVF isn’t just a buzzword; it’s a journey that’s helped millions of people welcome babies into their lives since the first “test-tube baby,” Louise Brown, was born in 1978. Today, it’s more advanced, more accessible, and packed with options to fit different needs. Whether you’re curious about the basics or digging into the nitty-gritty details, let’s dive into how IVF works, what it feels like, and what’s new in the world of fertility treatments as of April 2025.
What Is IVF, Anyway?
IVF stands for in vitro fertilization, which is a fancy way of saying “fertilization in a lab.” The word “vitro” comes from Latin, meaning “glass,” because the magic happens outside the body in a petri dish—not a test tube, despite the nickname! It’s part of a bigger family of treatments called assisted reproductive technology (ART), designed to help when natural conception isn’t happening.
Think of IVF as a teamwork project: doctors, eggs, sperm, and a lab all come together to create an embryo (a fertilized egg) that’s then placed into the uterus to grow into a baby. It’s used for all sorts of reasons—blocked fallopian tubes, low sperm count, unexplained infertility, or even to help same-sex couples or single parents build their families. The process has evolved a ton over the years, and today, it’s a go-to solution for about 2.5% of babies born in the U.S. each year.
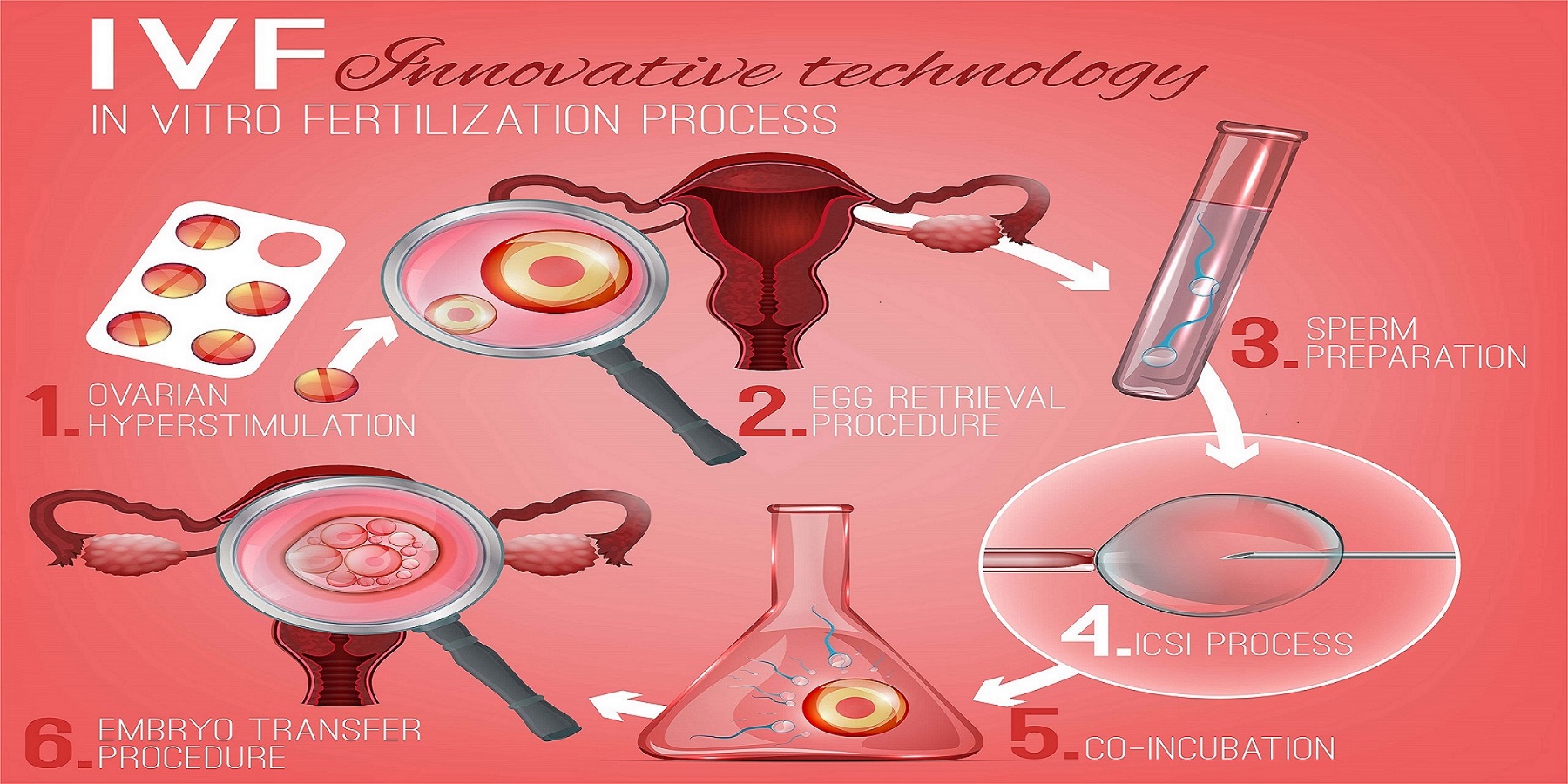
Step 1: Getting the Ovaries Ready with Stimulation
The IVF journey kicks off with a boost to the ovaries. Normally, your body releases one egg a month during ovulation, but IVF needs more players in the game. Doctors prescribe fertility drugs—usually injections you give yourself at home—to encourage the ovaries to produce multiple eggs at once. These meds, like follicle-stimulating hormone (FSH), trick your body into thinking it’s time to go big.
How It Works
For about 8-14 days, you’ll take these hormones while your doctor keeps an eye on things with ultrasounds and blood tests. The goal? To grow several healthy egg-containing sacs called follicles. It’s a bit like tending a garden—you water it, watch it grow, and wait for the perfect moment to harvest.
What It Feels Like
Some people breeze through this phase, while others feel bloated, moody, or tired. It’s not uncommon to feel like you’re on an emotional rollercoaster—hormones will do that to you! One mom described it as “feeling like a human pincushion” from all the shots, but said it was worth it when she saw her little one’s heartbeat later on.
Fresh Insight: Double Stimulation Trend
A newer twist in 2025 is something called dual stimulation. Instead of one round of egg production per cycle, some clinics now stimulate the ovaries twice in a single month. Research from the American Society for Reproductive Medicine (ASRM) shows this can double the number of eggs retrieved for women over 38, giving them a better shot at success without waiting another month. It’s not for everyone, but it’s a game-changer for those racing against the biological clock.
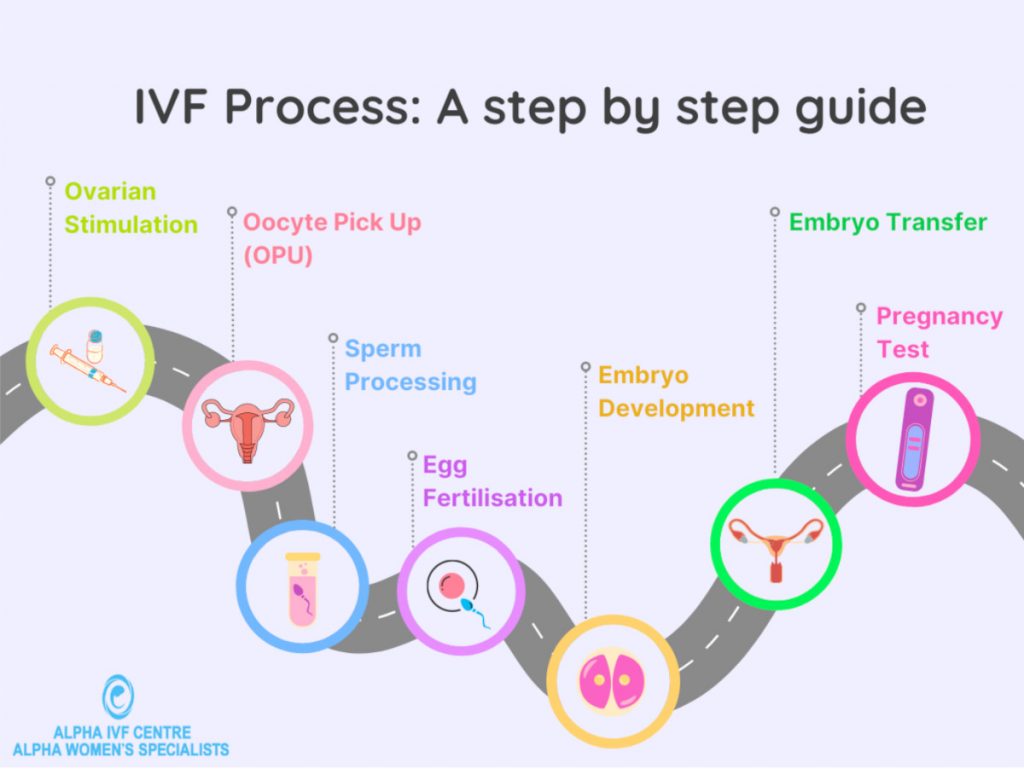
Step 2: Egg Retrieval—Harvesting the Goods
Once the follicles are plump and ready (usually about 15-20 millimeters in size), it’s time for egg retrieval. This is a quick procedure, done under light sedation, where a doctor uses a thin needle guided by ultrasound to pluck the eggs from your ovaries.
How It Works
Picture this: you’re snoozing comfortably while a tiny vacuum-like needle slips through your vaginal wall into each follicle, sucking out the eggs. It takes about 20-30 minutes, and you’re home the same day. Those eggs then head straight to the lab.
What to Expect
You might feel crampy or sore afterward, like a heavy period. Most people bounce back within a day or two. Fun fact: the average haul is 8-15 eggs, but it varies depending on age and health.
Pro Tip
✔️ Rest up post-retrieval—think cozy blankets and Netflix.
❌ Don’t plan a big workout; your ovaries need a break!
Unique Angle: Egg Quality Over Quantity
While many articles focus on how many eggs you get, experts in 2025 are buzzing about egg quality. A small study from Yale Fertility Center found that women who ate a diet rich in antioxidants (think berries, nuts, and leafy greens) for three months before IVF had fewer abnormal eggs. It’s not a guarantee, but it’s a simple tweak that could tip the scales.
Step 3: Sperm Meets Egg in the Lab
Now comes the star moment: fertilization. The eggs meet the sperm in a lab dish, and nature (with a little help) takes its course. There are two main ways this happens.
Option 1: Traditional IVF
Sperm and eggs are mixed together in a dish, and the strongest swimmers fertilize the eggs naturally. It’s like a mini Olympic race!
Option 2: ICSI (Intracytoplasmic Sperm Injection)
If sperm quality is low, a lab tech picks one healthy sperm and injects it directly into an egg. This is super common—about 70% of IVF cycles use ICSI, especially for male infertility.
What Happens Next
The fertilized eggs grow into embryos over 3-5 days. Lab pros watch them closely, looking for signs of healthy development—like the right number of cells dividing at the right pace.
Cool Update: Time-Lapse Imaging
A cutting-edge tool in 2025 is time-lapse embryo monitoring. Cameras snap pics of the embryos every few minutes, letting doctors spot the healthiest ones without disturbing them. A 2024 study from the University of California showed this boosts success rates by up to 15% compared to older methods. It’s like giving embryos a VIP screening!
Step 4: Embryo Transfer—Planting the Seed
After a few days, it’s time to put an embryo (or two) back into the uterus. This step is quick and painless—no sedation needed.
How It Works
A doctor threads a thin catheter through your cervix and releases the embryo into your uterus. It’s guided by ultrasound, so they can place it in the perfect spot. Then, you wait to see if it “sticks” and implants.
What It Feels Like
It’s like a Pap smear—mildly awkward but over fast. You might rest for a bit after, though studies say lying down for hours isn’t necessary. One patient said, “I felt hopeful but nervous, like waiting for a big test result.”
Interactive Moment: How Would You Prep?
Imagine you’re about to have an embryo transfer. Which would you do to stay calm?
- A) Meditate for 10 minutes
- B) Watch a funny movie
- C) Call a friend
Drop your pick in the comments—I’d love to hear!
Hidden Gem: The Frozen Advantage
Fresh embryo transfers used to be the norm, but frozen transfers are stealing the spotlight in 2025. Why? Freezing gives your body a break from hormones, and data from the CDC shows frozen transfers now have a 5-10% higher live birth rate for women under 35. Plus, you can save extra embryos for later—think of it as a backup plan for baby number two!
Step 5: The Two-Week Wait and Pregnancy Test
The next part is the hardest: waiting. About 10-14 days after the transfer, you’ll take a blood test to check for pregnancy hormones (hCG).
What’s Happening
If the embryo implants, it starts releasing hCG, signaling a pregnancy. If not, the cycle ends, and you and your doctor plan the next move.
Survival Tips
✔️ Keep busy—try a new hobby or binge a series.
❌ Avoid early home tests; they can give false hope or stress you out.
New Perspective: Emotional Support Matters
One thing rarely talked about is the mental toll of this wait. A 2024 survey by Resolve: The National Infertility Association found 60% of IVF patients felt isolated during this phase. Joining a support group—online or in-person—can make a huge difference. You’re not alone in this!

What Happens If It Works (Or Doesn’t)?
If the test is positive, congrats—you’re pregnant! You’ll start prenatal care like any other expecting parent. If it’s negative, it’s tough, but not the end. Many people need 2-3 cycles to succeed, and your doctor can tweak the plan based on what happened.
Success Rates by Age (2021 Data, Latest Available)
| Age Group | Live Birth Rate per Cycle |
|---|---|
| Under 35 | 50.8% |
| 35-37 | 32.4% |
| 38-40 | 20.1% |
| 41-42 | 9.7% |
| Over 42 | 7.9% |
Source: CDC Assisted Reproductive Technology Report
Fresh Take: Lifestyle Boosts
Beyond age, lifestyle tweaks can nudge success higher. A 2023 study from Harvard Medical School found that women who slept 7-9 hours nightly and cut caffeine to one cup a day had a 12% better chance of implantation. Small changes, big impact!
Risks and Realities of IVF
IVF isn’t all sunshine—it has risks worth knowing about.
Common Ones
- Ovarian Hyperstimulation Syndrome (OHSS): Overstimulated ovaries can swell and leak fluid. It’s rare (1-5% of cases) but can be serious.
- Multiple Births: Transferring more than one embryo ups the chance of twins, which carries higher risks like preterm birth.
- Ectopic Pregnancy: The embryo implants outside the uterus in 2-5% of cases.
Under-the-Radar Risk: Financial Strain
Here’s something not discussed enough: cost. A single cycle averages $15,000-$20,000 in the U.S., and insurance often doesn’t cover it. A 2025 report from the White House highlighted efforts to make IVF more affordable, like tax credits, but it’s still a hurdle. Some clinics now offer payment plans or “shared risk” programs where you get a refund if it fails after a set number of tries.
Who Can IVF Help?
IVF isn’t just for one type of person—it’s versatile.
Common Candidates
- Women with blocked or damaged fallopian tubes
- Men with low sperm count or motility
- Couples with unexplained infertility
- Same-sex couples or single parents using donors or surrogates
Emerging Use: Fertility Preservation
More people are freezing eggs or embryos before medical treatments like chemotherapy, which can harm fertility. A 2024 study from the Netherlands showed that 70% of women who froze eggs before cancer treatment later used them successfully. It’s like an insurance policy for your future family.
The Latest Buzz in IVF (April 2025)
IVF keeps evolving, and 2025 is no exception. Here’s what’s trending based on recent chatter on X and Google Trends.
AI-Powered Embryo Selection
Artificial intelligence is stepping in to pick the best embryos. A system called EmbryoScope uses AI to analyze growth patterns, boosting success rates by 10-20%, per a 2024 trial from UCSF. It’s like having a super-smart assistant in the lab.
Mini-IVF for Lower Costs
“Mini-IVF” uses fewer drugs to produce fewer eggs, cutting costs to $5,000-$7,000 per cycle. It’s gaining traction for younger women with good ovarian reserve, offering a budget-friendly option with solid results.
Reciprocal IVF for Same-Sex Couples
For female same-sex couples, reciprocal IVF—where one partner’s eggs are used and the other carries the pregnancy—is surging in popularity. Posts on X show couples celebrating this shared journey, blending science and love in a unique way.
Interactive Quiz: What’s Your IVF IQ?
Let’s test your knowledge! Answer these quick questions (no pressure—just fun):
- How long does a full IVF cycle usually take?
- A) 2 weeks
- B) 4-6 weeks
- C) 3 months
- What’s the most common reason for using ICSI?
- A) Low egg count
- B) Male infertility
- C) Older age
- True or False: Frozen embryos have lower success rates than fresh ones.
(Answers: 1-B, 2-B, 3-False. How’d you do? Share your score below!)
3 Things You Haven’t Heard About IVF
Most articles stick to the basics, but here are three under-the-radar topics that deserve more attention.
1. The Gut-Fertility Connection
Your gut health might play a role in IVF success. A 2024 study from the University of Toronto found that women with balanced gut microbiomes (think probiotics and fiber-rich diets) had a 15% higher implantation rate. It’s early research, but eating yogurt might just be your secret weapon.
2. Sperm DNA Fragmentation
For men, it’s not just about sperm count—DNA damage matters too. A 2023 paper from the ASRM showed that high sperm DNA fragmentation cuts success rates by 20%. New tests can check this, and antioxidants like vitamin C might help repair it. Ask your doc about it!
3. The Sibling Factor
Ever thought about using IVF for a second kid? Frozen embryos from your first cycle can make it easier (and cheaper) to grow your family later. A mom I spoke to used her leftovers from 2022 to welcome a second baby in 2025—no new egg retrieval needed. It’s like a two-for-one deal!
Your IVF Game Plan: Practical Tips
Ready to take the plunge? Here’s how to prep like a pro.
Before You Start
- Talk Money: Get a clear cost breakdown from your clinic—don’t be shy about asking for discounts or financing.
- Boost Health: Start a prenatal vitamin with folic acid and cut back on alcohol. For men, skip the hot tubs (heat hurts sperm!).
- Find Support: Line up a friend, therapist, or group to lean on. This ride’s smoother with a crew.
During the Process
- Track Meds: Use a phone app to remind you of shots—missing one can throw things off.
- Stay Hydrated: It helps with bloating and keeps you feeling human.
- Ask Questions: If something feels off, call your nurse. They’ve heard it all.
After the Transfer
- Chill Out: Light walks are fine, but skip the gym for a week.
- Eat Smart: Load up on protein and healthy fats—think eggs and avocado—to support implantation.
- Be Patient: Distract yourself during the wait. One couple I know painted their nursery to keep busy!
Real Stories, Real Hope
Sometimes, numbers and steps don’t tell the whole story. Take Sarah, a 36-year-old teacher from Iowa. After three failed IUIs, she tried IVF in 2024. “The shots were rough, and I cried a lot during the wait,” she said. “But holding my son now? I’d do it all again.” Or consider Mike and Jen, who used reciprocal IVF so Jen could carry Mike’s egg. “It felt like we both made her,” Mike shared on X last month. These stories remind us: IVF is tough, but the payoff can be everything.
Wrapping It Up: IVF Is a Journey Worth Exploring
IVF is more than a medical procedure—it’s a path to possibility. From stimulating eggs to transferring embryos, every step is a mix of science and heart. Sure, it’s got risks, costs, and waiting games, but it’s also got hope, innovation, and stories of triumph. Whether you’re just curious or seriously considering it, knowing how it works puts you in the driver’s seat.
What’s next? If IVF’s on your radar, chat with a fertility specialist. If not, share this with someone who might need it. And hey, drop a comment—what surprised you most about IVF? Let’s keep the conversation going!




