What Is the Live Birth Rate for IVF?
In vitro fertilization (IVF) has become a beacon of hope for millions of people dreaming of starting a family. If you’re exploring this option, you’ve probably heard a mix of success stories and uncertainties. One question stands out above the rest: What’s the live birth rate for IVF? It’s the number that can help you gauge your chances of holding a baby in your arms after this journey. Let’s dive into what this rate really means, how it varies, and what you can do to make sense of it for your own path.
This isn’t just about stats—it’s about understanding what’s possible for you. We’ll break it down with the latest research, real-world insights, and practical tips, all while keeping it simple and relatable. Whether you’re just curious or ready to take the plunge, here’s everything you need to know about IVF live birth rates in 2025.
Why the Live Birth Rate Matters
The live birth rate is the golden metric in IVF. It tells you the percentage of IVF cycles that result in a baby born alive. Unlike pregnancy rates, which only confirm a positive test, the live birth rate cuts through the noise to focus on the endgame: bringing a child home. For anyone considering IVF, this number offers a reality check and a starting point for planning.
But here’s the catch—it’s not a one-size-fits-all figure. Your age, health, and even where you live can shift the odds. In 2021, the UK’s Human Fertilisation and Embryology Authority (HFEA) reported that about 25% of IVF cycles using a patient’s own fresh eggs led to a live birth. Fast forward to today, and advancements have nudged that number up slightly, but it’s still a rollercoaster of variables. So, what’s behind these numbers? Let’s unpack it.
How IVF Live Birth Rates Are Calculated
The live birth rate isn’t some mysterious guess—it’s a carefully tracked statistic. Clinics measure it by dividing the number of live births by the total number of IVF cycles started in a given time. A “cycle” here means one round of treatment, from ovarian stimulation to embryo transfer. If frozen embryos are used later, those transfers might count as part of the original cycle or as separate ones, depending on how the data’s reported.
For example, if a clinic starts 100 cycles and 30 result in a live birth, the rate is 30%. Simple, right? Not quite. The rate can shift based on:
- Fresh vs. Frozen Embryos: Frozen embryo transfers have been gaining ground, often showing higher success rates because embryos can be transferred when your body’s in peak condition.
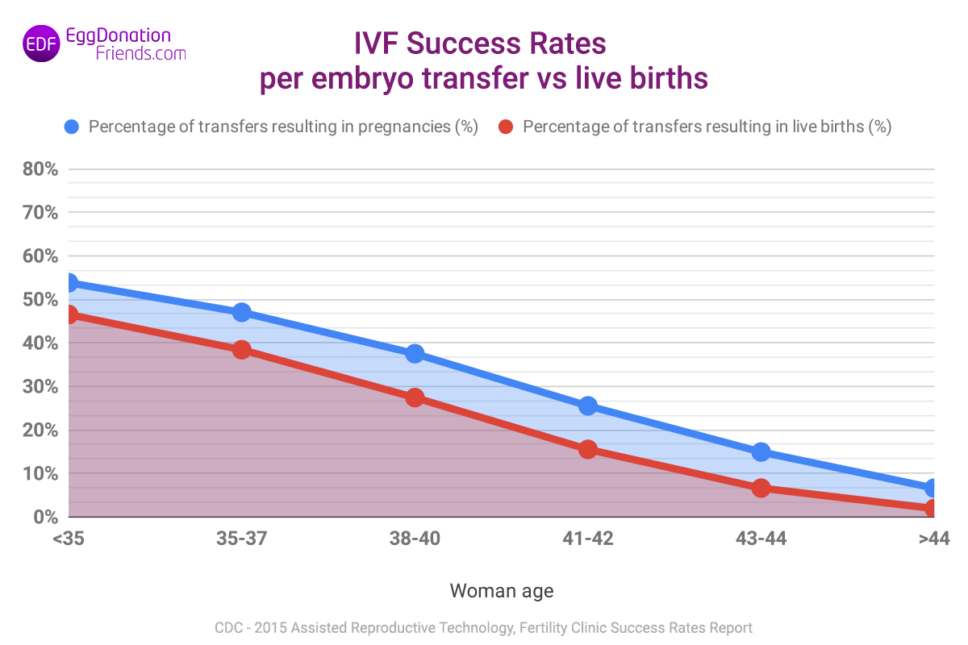
- Age Groups: Younger patients (under 35) typically see rates around 40-50%, while those over 40 might dip below 10%.
- Cycle Count: Some stats look at one cycle, while others track “cumulative” rates over multiple tries.
The Society for Assisted Reproductive Technology (SART) in the U.S. and the HFEA in the UK publish annual reports with these breakdowns. In 2022, SART noted that for women under 35, the live birth rate per egg retrieval was about 51%. That’s encouraging—but it’s just one piece of the puzzle.
What’s the Average Live Birth Rate for IVF in 2025?
As of April 2025, IVF success rates have seen steady improvement thanks to better technology and techniques. Based on the latest data trends from sources like the CDC and HFEA, here’s a snapshot of what you might expect:
- Under 35: Around 45-50% per cycle with fresh embryos; up to 55% with frozen ones.
- 35-37: About 35-40% per cycle, with frozen transfers slightly higher.
- 38-40: Roughly 25-30%, dropping as age climbs.
- Over 40: 10-15% with your own eggs, but closer to 30-35% with donor eggs.
These are averages, not guarantees. A 2023 study in Human Reproduction found that cumulative live birth rates—your odds after multiple cycles—can hit 65% for women under 40 after six tries. That’s a big jump from a single cycle, showing persistence can pay off.
But numbers alone don’t tell the whole story. Your clinic’s expertise, your specific diagnosis (like low ovarian reserve or male factor infertility), and even lifestyle factors play huge roles. Let’s explore what shapes these odds.
Factors That Influence IVF Live Birth Rates
IVF isn’t a magic wand—it’s a science shaped by biology and circumstance. Here’s what can tip the scales:
Age: The Biggest Player
Your age is the single biggest factor. Eggs naturally decline in quality and quantity as you get older. For women under 35, the odds are strong because their eggs are more likely to form healthy embryos. By 40, that chance drops sharply. A 2024 report from the CDC showed that women over 42 using their own eggs had a live birth rate of just 4% per cycle. Compare that to donor egg cycles, where rates hold steady at 30-40% regardless of the recipient’s age.
Embryo Quality
Not all embryos are created equal. Clinics grade them based on appearance and development—think of it like picking the ripest fruit. Higher-quality embryos (blastocysts, for instance) have a better shot at implanting and growing. Preimplantation genetic testing (PGT) can boost success by screening for chromosomal issues, though it’s not foolproof.
Lifestyle Choices
Smoking, excess weight, and stress aren’t just buzzkills—they can lower your IVF odds. A 2023 study in Fertility and Sterility found that women with a BMI over 30 had a 10% lower live birth rate than those in a healthy range. Cutting back on caffeine and getting regular exercise? That’s a small but real edge.
Clinic Expertise
Where you go matters. Top-tier clinics with advanced labs and experienced staff often report higher success rates. The HFEA’s 2022 data showed a 5-10% gap between the best and average UK clinics. Check your clinic’s track record—it’s your starting line.
Number of Cycles
One try might not cut it. Cumulative rates climb with each cycle, peaking around 3-6 attempts for most. A UK study from 2015 (still relevant today) found that women aged 40-42 hit a 31.5% cumulative rate after six cycles. Patience can be a game-changer.
Fresh vs. Frozen: Which Wins?
Here’s a debate you might not see coming: fresh embryo transfers vs. frozen ones. In the past, fresh was king—transferring embryos right after egg retrieval felt like the natural choice. But frozen transfers are stealing the spotlight.
Why? Freezing lets doctors time the transfer to your body’s peak readiness, avoiding overstimulation from hormones. In 2022, the HFEA reported frozen embryo transfers had a 31% live birth rate per transfer for women under 35, compared to 28% for fresh. That gap widens with age. Plus, freezing means you can bank embryos for later, spreading out your chances.
Quick Tip: Ask your doctor about “freeze-all” cycles if you’re worried about hormone overload. It’s a strategy gaining traction for a reason.
Donor Eggs: A Game-Changer for Older Parents
If you’re over 40 and using your own eggs feels like a long shot, donor eggs might be your ace. The live birth rate with donor eggs hovers around 35-40% per cycle, no matter the recipient’s age. Why? Younger donor eggs (usually from women in their 20s) are more likely to form viable embryos.
Take Sarah, a 43-year-old from California. After three failed cycles with her own eggs, she switched to a donor and welcomed twins in 2024. Her story’s not rare—donor egg IVF accounts for about 10% of U.S. cycles, per SART, and it’s a lifeline for many.
Consider This: Donor eggs come with emotional and ethical layers. It’s worth talking to a counselor to see if it fits your vision.

Interactive Quiz: What’s Your IVF Starting Point?
Let’s make this personal. Answer these quick questions to get a rough sense of where you stand:
- How old are you?
- A) Under 35
- B) 35-40
- C) Over 40
- Are you using your own eggs or donor eggs?
- A) My own
- B) Donor
- How many cycles are you willing to try?
- A) Just 1
- B) 2-3
- C) 4 or more
Results:
- Mostly A’s: You’re in a strong spot—rates could hit 40-50% per cycle.
- Mix of A and B: Solid odds, especially with donor eggs or multiple tries (30-40%).
- Mostly C’s: It’s tougher, but donor eggs or persistence could lift you to 20-35% cumulatively.
This isn’t a diagnosis—just a nudge to talk to your doctor with clearer eyes.
Beyond the Numbers: What’s Not Talked About Enough
Most articles stop at stats and basic tips. But there’s more to IVF than percentages. Here are three angles you won’t find everywhere:
The Emotional Toll of “Success”
Even a 50% live birth rate means half the time, you’re facing disappointment. Studies show 1 in 3 IVF patients experience anxiety or depression during treatment. Yet, clinics rarely talk about mental prep. Journaling, support groups, or a therapist can be as vital as any injection.
Try This: Write down one thing you’re grateful for each day of your cycle. It’s small, but it builds resilience.
The Hidden Costs of Multiple Cycles
IVF isn’t cheap—$12,000-$15,000 per cycle in the U.S., per the American Society for Reproductive Medicine (ASRM). Cumulative success sounds great, but can you afford six rounds? Insurance coverage varies wildly, and only 19 states mandate some fertility help as of 2025. Dig into grants or financing early—it’s a lifeline not enough people explore.
Environmental Factors: The New Frontier
Emerging research hints that air pollution and chemical exposure might dent IVF success. A 2024 study in Environmental Health Perspectives found women in high-pollution areas had a 5-7% lower live birth rate. It’s early days, but living cleaner—think air purifiers or organic diets—could be a quiet boost.
Boosting Your IVF Odds: Practical Steps
You can’t control everything, but you can stack the deck. Here’s how:
✔️ Optimize Your Health: Aim for a BMI of 19-25, quit smoking, and limit alcohol. A 2023 meta-analysis showed these tweaks lift rates by up to 15%.
✔️ Choose the Right Clinic: Look at SART or HFEA data for clinics with above-average rates in your age group. Visit in person—vibes matter.
✔️ Consider PGT: Testing embryos for genetic issues can bump success by 10-20%, especially if you’re over 35.
❌ Don’t Rush: Skipping rest between cycles can stress your body. Give it 1-2 months if possible.
❌ Avoid Overloading on Supplements: CoQ10 and DHEA might help egg quality, but more isn’t better—stick to doctor-approved doses.
Step-by-Step Plan:
- Get a full fertility workup (hormone levels, sperm analysis, etc.).
- Pick a clinic with a strong track record for your situation.
- Build a 3-month prep plan—diet, exercise, stress relief.
- Discuss fresh vs. frozen and PGT with your team.
- Set a budget and cycle limit upfront.
Real Stories: What IVF Success Looks Like
Numbers are great, but people bring them to life. Meet Lisa, a 37-year-old teacher from Texas. After two miscarriages, she tried IVF in 2023. Her first cycle failed, but a frozen transfer in 2024 gave her a son. “It was the waiting that killed me,” she says. “But knowing the odds kept me grounded.”
Then there’s Mark and Jen, both 32, who faced male infertility. Three cycles later, with ICSI (a sperm injection tweak), they welcomed a daughter last month. “We didn’t expect it to take so long,” Mark admits, “but the clinic’s honesty about rates helped us push through.”
These aren’t outliers—they’re proof the stats play out in real homes.
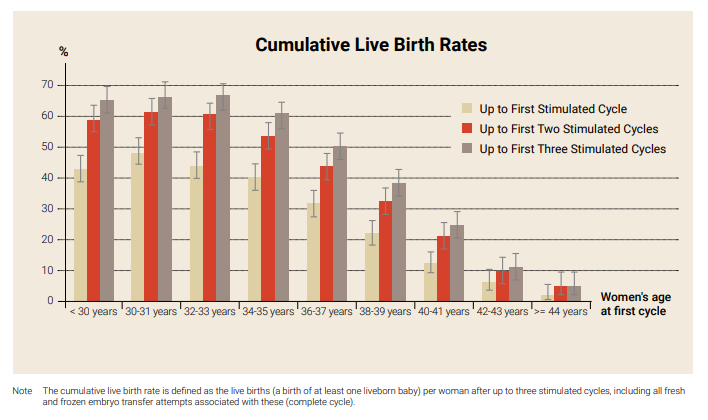
Cumulative Success: The Long Game
One cycle’s not the whole story. Cumulative live birth rates—your odds over multiple tries—paint a fuller picture. A 2023 UK study showed:
| Age Group | 1 Cycle | 3 Cycles | 6 Cycles |
|---|---|---|---|
| Under 35 | 48% | 68% | 77% |
| 35-37 | 39% | 58% | 65% |
| 38-40 | 27% | 45% | 52% |
| 40-42 | 12% | 25% | 31% |
Over 42? Rates plateau around 10-15% with your own eggs, but donor eggs keep climbing. The takeaway? If you can handle the time and cost, sticking with it often pays off.
Poll: What’s Your IVF Priority?
Let’s hear from you! Pick one:
- A) Highest live birth rate, whatever it takes.
- B) Lowest cost, even if it means fewer tries.
- C) Emotional support through the process.
Drop your choice in the comments—it’s a quick way to see what drives others too.
The Future of IVF Live Birth Rates
What’s next? IVF’s evolving fast. In 2025, we’re seeing:
- AI-Powered Embryo Selection: Algorithms are picking winners with 5-10% better accuracy than human eyes, per a Nature study.
- Milder Stimulation: Less intense hormone protocols are cutting risks and boosting rates for some.
- Gene Editing Buzz: Not here yet, but CRISPR talk is heating up—ethical debates included.
These could push live birth rates higher, especially for tougher cases. Stay tuned—your options might look different in a year.
Wrapping It Up: Your IVF Roadmap
So, what’s the live birth rate for IVF? It’s a moving target—40-50% for the young and healthy, 10-15% for the over-40 crowd, and a solid 35% with donor eggs. But it’s more than a number. It’s about your body, your choices, and your grit. Armed with the latest data and a few insider tips, you’re ready to ask the right questions and chart your course.
Think of IVF like planting a garden. Some seeds sprout fast, others need more time, and a few need extra care. You’ve got the tools to tend it—now it’s about finding your rhythm. Talk to your doctor, lean on your people, and take it one step at a time. Your odds? They’re yours to shape.




