What Is the Success Rate of IVF?
In vitro fertilization (IVF) has been a game-changer for millions of people dreaming of starting a family. If you’re reading this, chances are you’re curious about how successful IVF really is. Maybe you’re weighing your options, or perhaps you’re just fascinated by the science behind it. Either way, you’re in the right place! IVF success rates can feel like a puzzle—numbers shift depending on age, health, and a dozen other factors. Let’s break it down together, step by step, with the latest insights, practical tips, and a few surprises that most articles skip over.
IVF isn’t a one-size-fits-all solution, but it’s helped over 10 million babies come into the world since the first “test-tube baby,” Louise Brown, was born in 1978. That’s a lot of happy parents! Still, success isn’t guaranteed, and the journey can feel like an emotional rollercoaster. So, what’s the real deal with IVF success rates? How do they stack up for different people, and what can you do to boost your odds? Grab a comfy seat—we’re diving deep into the numbers, the science, and the stories behind IVF.
Understanding IVF: A Quick Rundown
Before we get into success rates, let’s make sure we’re on the same page about what IVF actually is. IVF stands for in vitro fertilization, which means “fertilization in glass.” It’s a process where doctors take eggs from the ovaries, mix them with sperm in a lab, and then place the resulting embryo (or embryos) into the uterus. The goal? A healthy pregnancy.
The process usually takes a few weeks per cycle and involves several steps: stimulating the ovaries to produce multiple eggs, retrieving those eggs, fertilizing them, growing the embryos, and transferring them. It’s high-tech, sure, but it’s also a blend of art and science that’s been fine-tuned over decades.
Why do people turn to IVF? Sometimes it’s because of blocked fallopian tubes, low sperm count, or conditions like endometriosis. Other times, it’s unexplained infertility or a desire to freeze embryos for later. Whatever the reason, the big question remains: how often does it work?
The Big Picture: What Are IVF Success Rates?
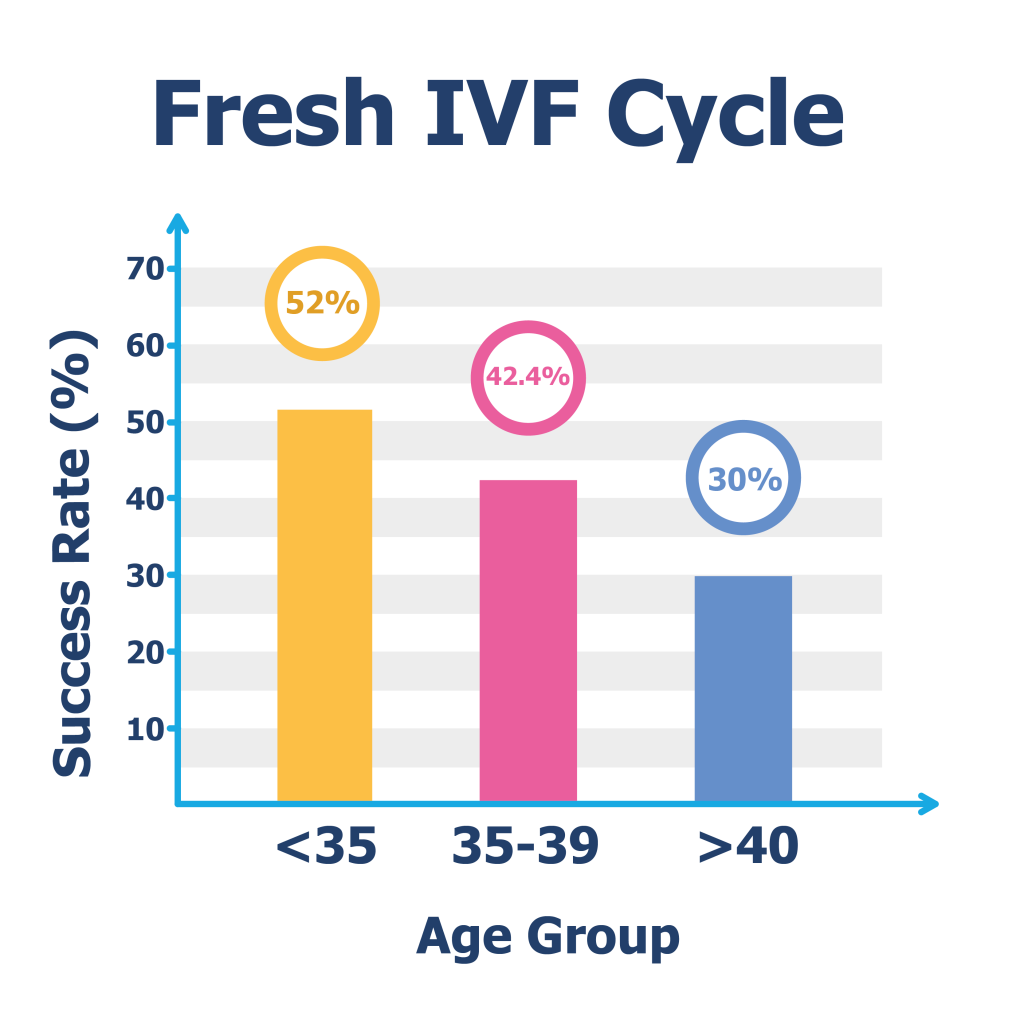
Success in IVF is usually measured by the “live birth rate”—the percentage of cycles that result in a baby being born. According to the latest data from the Centers for Disease Control and Prevention (CDC), about 1 in 3 IVF cycles leads to a live birth when using fresh embryos from a woman’s own eggs. But here’s the catch: that number changes a lot depending on who you are and what you’re working with.
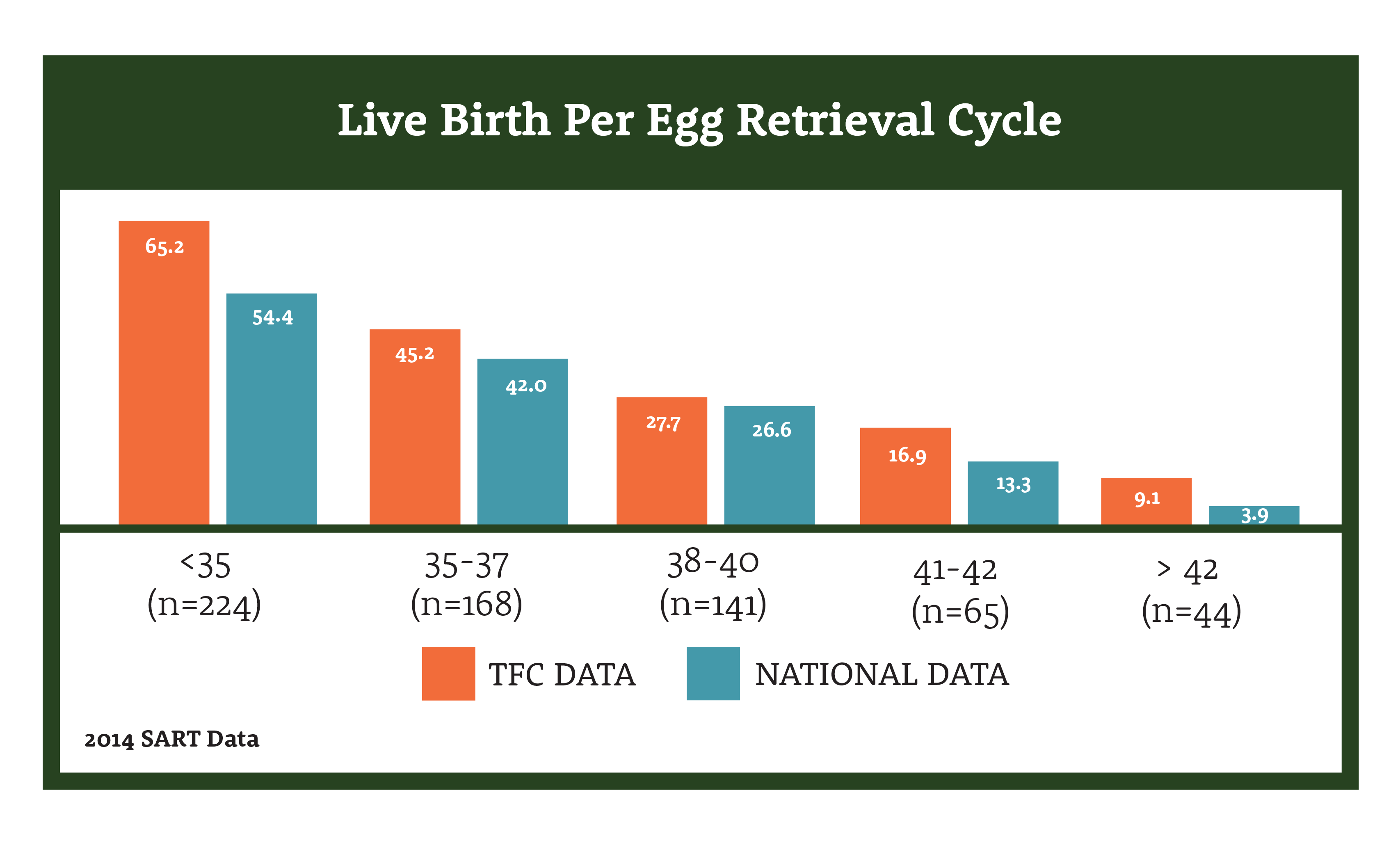
For example, the Society for Assisted Reproductive Technology (SART) tracks outcomes across the U.S. Their 2021 data shows that for women under 35, the live birth rate per egg retrieval is around 50%. For women over 40, it drops to about 7-10%. Age is a huge factor, but it’s not the only one. Things like egg quality, sperm health, and even the clinic you choose play a role.
Here’s a quick snapshot based on SART’s 2021 stats:
| Age Group | Live Birth Rate per Egg Retrieval |
|---|---|
| Under 35 | 50.2% |
| 35-37 | 38.1% |
| 38-40 | 24.5% |
| 41-42 | 11.8% |
| Over 42 | 4.1% |
These numbers might look intimidating, but they’re just averages. Your personal odds could be higher—or lower—depending on your situation. Let’s unpack what drives these rates and how you can tilt the scales in your favor.
Why Age Matters So Much
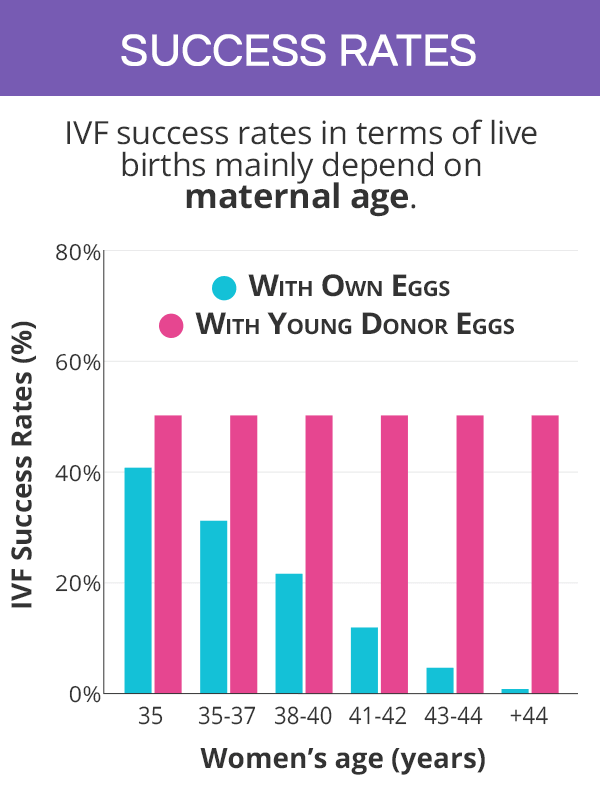
If there’s one thing you’ll hear over and over about IVF, it’s that age is a big deal. Why? Because a woman’s eggs age along with her, and older eggs are less likely to turn into healthy embryos. By the time you hit your late 30s, both the quantity and quality of eggs start to decline. It’s biology, not judgment!
For women under 35, the odds are pretty good—about half of IVF cycles lead to a baby. But after 40, the success rate drops sharply. That’s not to say it’s impossible—plenty of women over 40 have babies with IVF, especially if they use donor eggs. In fact, donor egg IVF can boost success rates to 50-60% per cycle, no matter the woman’s age, because the eggs come from someone younger (usually in their 20s or early 30s).
What This Means for You
- Under 35? You’re in the sweet spot. Your body’s more likely to respond well to fertility drugs, and your eggs are typically top-notch.
- 35-40? Success is still very possible, but you might need more cycles or extra tweaks like genetic testing of embryos.
- Over 40? Don’t lose hope! Donor eggs or advanced techniques could be your golden ticket.
Age isn’t the whole story, though. Let’s look at what else shapes your chances.
Beyond Age: Other Factors That Affect IVF Success
IVF success isn’t just about how old you are—it’s about your unique body and circumstances. Here are some key players that can make or break your odds:
1. Egg and Sperm Quality
Healthy eggs and sperm are the building blocks of a good embryo. If either is struggling (say, low sperm motility or poor egg quality due to conditions like polycystic ovary syndrome), success rates can dip. The good news? Techniques like intracytoplasmic sperm injection (ICSI)—where a single sperm is injected into an egg—can help when sperm quality is an issue.
2. Uterine Health
The uterus is where the embryo needs to implant and grow. Problems like fibroids, scar tissue, or a thin uterine lining can lower your chances. Doctors often check this with an ultrasound or hysteroscopy before starting IVF.
3. Lifestyle Choices
Smoking, heavy drinking, and being significantly over- or underweight can hurt your odds. A 2022 study in Human Reproduction found that women with a BMI between 19 and 30 had higher success rates than those outside that range. Small changes—like cutting back on caffeine or hitting the gym—can make a difference.
4. Number of Embryos Transferred
Transferring more embryos might seem like a way to up your chances, but it’s a double-edged sword. It increases the odds of pregnancy, sure, but also the risk of twins or triplets, which can bring complications. Most clinics now recommend single embryo transfer (SET) to keep things safer.
5. Clinic Expertise
Not all IVF clinics are created equal. A top-notch lab with experienced embryologists can boost your success rate by 5-10%, according to a 2023 report from the American Society for Reproductive Medicine (ASRM). Picking the right clinic is like choosing a chef for your favorite meal—skill matters.
Fresh vs. Frozen Embryos: Which Wins?
Here’s something you might not have thought about: whether you use fresh or frozen embryos can affect your success rate. In the past, fresh embryo transfers were the go-to, but frozen embryo transfers (FET) are stealing the spotlight.
Why? Freezing embryos lets your body recover from the egg retrieval process, and it allows doctors to time the transfer perfectly with your uterine lining. A 2024 study in Fertility and Sterility found that FET success rates are now slightly higher than fresh transfers—around 40% vs. 35% per cycle for women under 38. Plus, freezing means you can save extra embryos for later, giving you more shots at success without starting from scratch.
Fresh vs. Frozen: A Quick Comparison
- Fresh Transfers
- ✔️ Faster process (no waiting to freeze/thaw)
- ❌ Higher risk of ovarian hyperstimulation syndrome (OHSS)
- Frozen Transfers
- ✔️ Better timing for implantation
- ❌ Slightly more expensive due to storage fees
Which is best for you? It depends on your body and your doctor’s advice. More clinics are leaning toward frozen these days, and the data backs them up.
Boosting Your IVF Odds: Practical Tips
Okay, so success rates vary—got it. But what can you do to improve your chances? Plenty! Here are some actionable steps grounded in science and real-world experience:
Step 1: Optimize Your Health
- Eat a balanced diet rich in antioxidants (think berries, nuts, and leafy greens).
- Aim for 30 minutes of moderate exercise most days—yoga or brisk walks are great.
- Quit smoking and limit alcohol to 1-2 drinks per week, max.
Step 2: Pick the Right Clinic
- Look at SART or CDC success rates for clinics near you.
- Ask about their lab tech—do they use cutting-edge tools like time-lapse imaging?
- Check patient reviews for a vibe on bedside manner and support.
Step 3: Consider Add-Ons Wisely
Some clinics offer extras like preimplantation genetic testing (PGT) to screen embryos for chromosomal issues. A 2023 study in The Lancet showed PGT can bump live birth rates by 10-15% for women over 35. But beware—add-ons like acupuncture or endometrial scratching lack solid proof, so don’t waste money unless your doctor sees a clear benefit.
Step 4: Manage Stress
IVF can feel like an emotional marathon. Meditation, therapy, or even a good laugh with friends can keep you grounded. A 2022 study from the University of California found that lower stress levels correlated with a 7% higher implantation rate.
Interactive Quiz: What’s Your IVF Knowledge?
Let’s take a quick break—how much do you know about IVF success? Answer these questions and see!
- What’s the biggest factor in IVF success?
- A) Clinic location
- B) Age
- C) Number of doctors
- True or False: Frozen embryos always work better than fresh ones.
- A) True
- B) False
- Which lifestyle change can boost your odds?
- A) Drinking more coffee
- B) Quitting smoking
- C) Sleeping less
Answers: 1) B, 2) B (it depends!), 3) B. How’d you do? Share your score with a friend or in your head—bragging rights are free!
The Emotional Side: What Numbers Don’t Tell You
Success rates are great, but they don’t capture the full IVF experience. For every 50% statistic, there’s a couple holding their breath during the two-week wait, or a solo parent celebrating a faint pink line. IVF is as much about hope as it is about science.
Take Sarah, a 37-year-old teacher I heard about through a fertility support group. After two failed cycles, she switched clinics, adjusted her diet, and used PGT. Her third try worked—she’s now mom to a spunky toddler. Then there’s Mark and Lisa, who faced male infertility. ICSI gave them twins after just one cycle. These stories remind us: stats are a starting point, not the whole journey.
On the flip side, not every cycle ends in a baby. About 1 in 4 pregnancies from IVF ends in miscarriage, especially for older women. That’s tough, but it’s also why support—whether from a partner, counselor, or online community—matters so much.
Donor Eggs: A Game-Changer for Older Parents
If you’re over 40 and worried about low success rates, donor eggs might be worth a look. Using eggs from a younger donor (usually 21-34 years old) can skyrocket your chances to 50-60% per cycle, according to the CDC. It’s not for everyone—some folks want a genetic connection—but it’s a powerful option.
What’s it like? You pick a donor (anonymous or known), the eggs are fertilized with your partner’s sperm (or donor sperm), and the embryo goes into your uterus. The baby won’t share your DNA, but you’ll carry and deliver them. It’s a unique path to parenthood that’s growing in popularity—about 10% of IVF cycles in the U.S. now use donor eggs.
The Latest Trends: What’s New in IVF?
IVF isn’t standing still. Here are three cutting-edge developments that could shake up success rates in the next few years:
1. Artificial Intelligence in Embryo Selection
AI is helping embryologists pick the best embryos by analyzing thousands of images in seconds. A 2024 trial in Nature Medicine found AI-boosted selection improved live birth rates by 12% compared to human-only methods. It’s like having a super-smart assistant in the lab!
2. In Vitro Gametogenesis (IVG)
This is wild—scientists are working on turning skin cells into eggs or sperm. It’s still experimental (mostly in mice), but if it works in humans, it could help people who can’t produce gametes naturally. Imagine a future where infertility is just a speed bump!
3. Microfluidics
Tiny devices that mimic the body’s natural environment are making embryo culture more precise. A 2023 study in Reproductive Biology showed microfluidic systems increased embryo quality by 15%. It’s not widespread yet, but it’s a peek at IVF’s high-tech future.
IVF Around the World: How Do We Compare?
Success rates aren’t the same everywhere. In the U.S., the average live birth rate per cycle hovers around 30-35%. In Europe, countries like Denmark lead with rates near 40%, thanks to generous insurance coverage and top-tier clinics. Meanwhile, in places like India, costs are lower (around $3,000 per cycle vs. $12,000 in the U.S.), but success rates vary widely depending on the facility.
What’s driving the differences? Access to technology, doctor training, and how many embryos clinics transfer. In the UK, single embryo transfers are the norm, keeping multiple births low (4% in 2022, per HFEA) while still hitting solid success rates.
Poll Time: What’s Your IVF Priority?
Let’s get interactive again! If you were doing IVF, what would matter most to you? Pick one:
- A) Highest success rate, no matter the cost
- B) Lowest cost, even if it takes more tries
- C) Fewest side effects from meds
- D) Emotional support during the process
Think about it—what’s your top pick? Jot it down or share it with someone. It’s a great way to clarify what you value most.
Three Things You Haven’t Heard About IVF Success
Most articles stick to the basics—age, embryos, clinics. But here are three under-the-radar factors that can sway your IVF outcome:
1. The Day of Embryo Transfer
Embryos are usually transferred on day 3 or day 5 (blastocyst stage). Day 5 transfers have a higher success rate—around 45% vs. 35% for day 3, per a 2023 ASRM report. Why? Blastocysts are more developed, so doctors can better spot the strong ones. If your clinic pushes day 3, ask why—it might not be the best call.
2. Your Vitamin D Levels
Low vitamin D is linked to lower implantation rates. A 2022 study in Journal of Clinical Endocrinology found women with optimal levels (30-50 ng/mL) had a 9% higher success rate. Get a simple blood test and talk to your doctor about supplements if you’re low.
3. Sperm DNA Fragmentation
Even if sperm count looks fine, damaged DNA can tank embryo quality. A 2024 study in Andrology showed that high fragmentation cuts success rates by 20%. Tests aren’t routine, but if you’ve had repeat failures, ask your doc to check it.
These nuggets don’t get enough airtime, but they could be the edge you need.
A Simple Calculation: Your Personal Odds
Want a rough idea of your chances? Here’s a back-of-the-envelope way to estimate, based on CDC and SART data:
- Start with your age group’s baseline (e.g., 50% for under 35, 25% for 38-40).
- Add 5-10% if you’re in great health (normal BMI, no smoking).
- Subtract 5-10% if you’ve got challenges like endometriosis or low ovarian reserve.
- Add 10-15% if you’re using PGT or a top clinic.
Example: A 36-year-old in good health at a great clinic might estimate 38% (base) + 10% (health/clinic) = 48% per cycle. It’s not exact, but it’s a starting point. Chat with your doctor for a real prediction.




