What’s IVF? Your Complete Guide to In Vitro Fertilization
In vitro fertilization, or IVF, is a term you might’ve heard tossed around in conversations about starting a family, especially when things don’t go as planned. It’s a process that’s helped millions of people become parents, but it’s also surrounded by questions, myths, and a bit of mystery. If you’re curious about what IVF really is, how it works, and whether it might be an option for you or someone you know, you’re in the right place. This guide is here to break it all down—step by step, in a way that’s easy to follow and packed with the latest info you won’t find everywhere else.
IVF isn’t just a medical procedure; it’s a journey. It’s about hope, science, and sometimes a little bit of patience. Whether you’re dealing with fertility challenges, exploring options as a single person or same-sex couple, or just want to understand this incredible technology, let’s dive into what makes IVF tick.
What Does IVF Actually Mean?
IVF stands for in vitro fertilization. The phrase “in vitro” comes from Latin and means “in glass,” which gives you a clue about how it works. Unlike natural conception, where a sperm fertilizes an egg inside the body, IVF happens outside—in a lab dish. Scientists take eggs from the ovaries, mix them with sperm, and if everything goes well, an embryo forms. That embryo is then placed back into the uterus to grow into a baby.
Think of it like giving nature a helping hand. Instead of waiting for the stars to align inside the body, doctors create the perfect conditions in a lab. It’s been around since 1978, when the first “test-tube baby,” Louise Brown, was born in England. Since then, over 8 million babies worldwide have come into the world thanks to IVF.
But it’s not just for couples who can’t conceive naturally. IVF is also used by people freezing their eggs for the future, same-sex couples building families, or those avoiding genetic conditions. It’s a tool with a lot of possibilities—and a lot of heart.
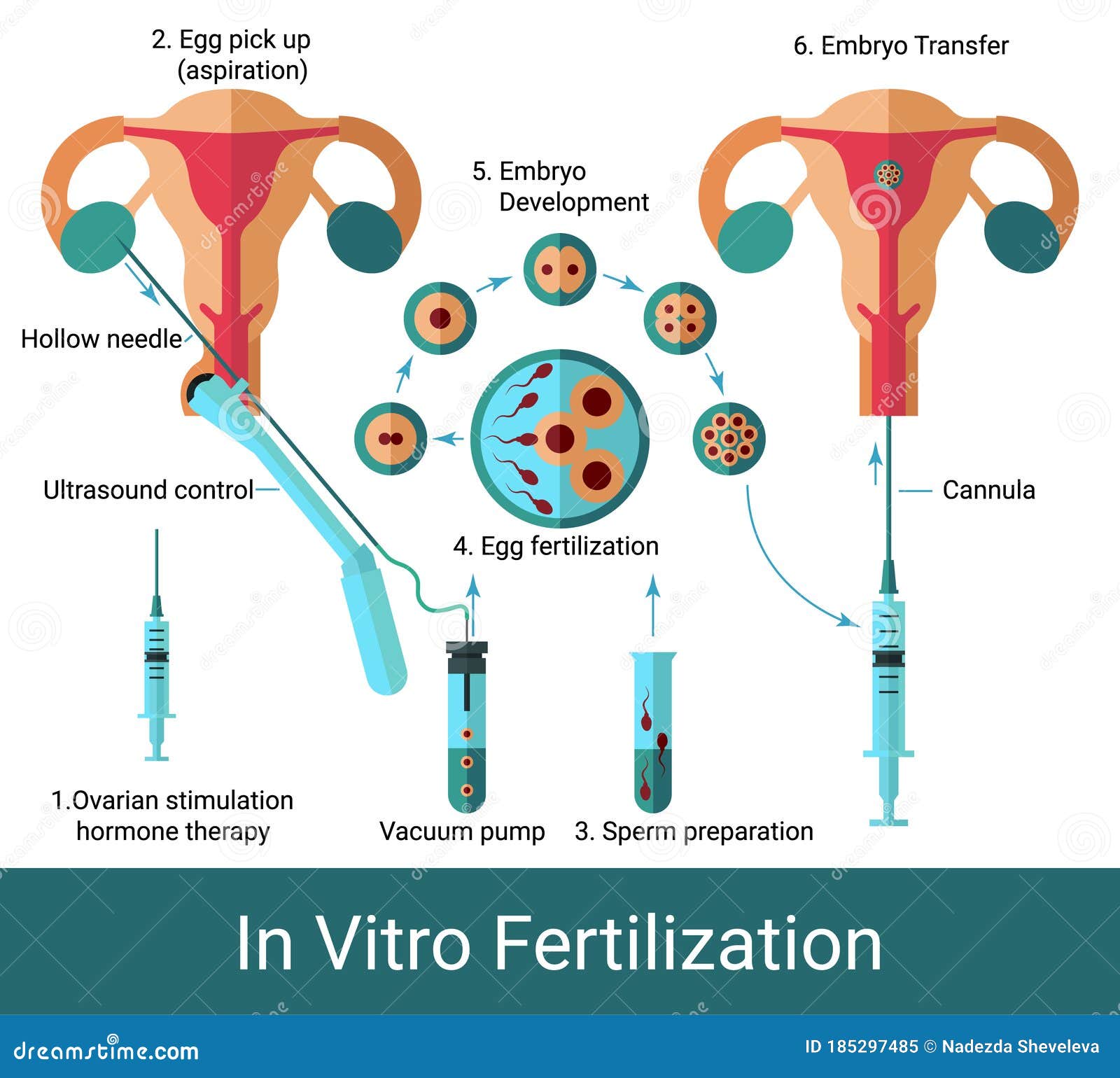
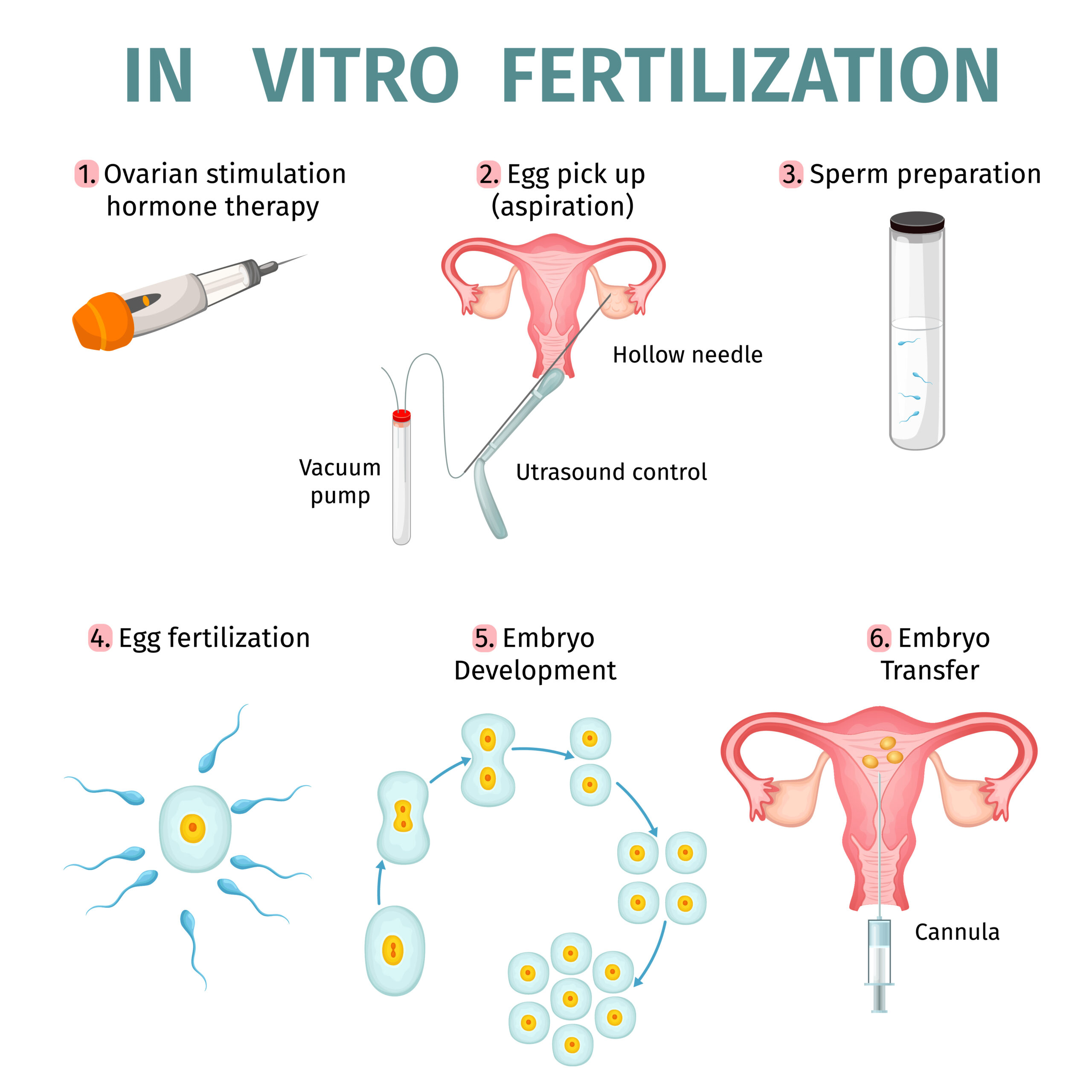
How Does IVF Work? A Step-by-Step Look
IVF might sound complicated, but it’s really a series of clear steps. Here’s what happens, explained like a roadmap to parenthood:
Step 1: Boosting Egg Production
Normally, your ovaries release one egg a month. With IVF, doctors want more chances for success, so they use fertility drugs to kick things into high gear. These meds—usually shots you give yourself—tell your ovaries to produce several eggs at once. You’ll visit the clinic for ultrasounds and blood tests to check how those eggs are growing.
Step 2: Collecting the Eggs
Once the eggs are ready (about 10-14 days later), it’s time to get them out. This is called egg retrieval. A doctor uses a thin needle, guided by ultrasound, to gently pull the eggs from your ovaries. Don’t worry—you’re asleep under light sedation, so it’s painless. It takes about 20 minutes, and you’re back home the same day.
Step 3: Fertilizing the Eggs
Now the lab magic happens. The eggs meet the sperm in a dish. Sometimes, the sperm just swims up and does its thing (standard IVF). Other times, if the sperm needs a nudge, a scientist picks the healthiest one and injects it directly into the egg (a method called ICSI—intracytoplasmic sperm injection). After a day or two, you’ll know if embryos have formed.
Step 4: Growing the Embryos
The embryos chill in the lab for 3-5 days, growing stronger. Scientists keep an eye on them, grading their quality. The best ones—usually those that reach the blastocyst stage by day 5—get the green light for the next step.
Step 5: Transferring the Embryo
This is the big moment. A doctor uses a thin tube to place one or two embryos into your uterus. It’s quick, like a Pap smear, and you’re awake for it. If an embryo sticks to the uterine lining (implantation), pregnancy begins. About 10-14 days later, a blood test confirms if it worked.
Step 6: What About Extras?
If there are leftover embryos, you can freeze them for later. This is super common—about 40% of IVF cycles involve frozen embryos, and they often have just as good a shot at success.
It’s a process that takes about 4-6 weeks per cycle, but every step is carefully planned to boost your odds.
Who Can IVF Help?
IVF isn’t a one-size-fits-all solution—it’s a lifeline for lots of different people. Here’s who might turn to it:
- Couples with Infertility: Blocked fallopian tubes, low sperm count, or unexplained struggles after a year of trying? IVF can bypass those hurdles.
- Older Parents: As women age, egg quality drops. IVF can use donor eggs or help retrieve what’s left for a better shot.
- Same-Sex Couples and Single Folks: With donor sperm, eggs, or surrogates, IVF opens doors to parenthood.
- People with Genetic Risks: If you carry a condition like cystic fibrosis, IVF with genetic testing (called PGT) can screen embryos to avoid passing it on.
- Fertility Preservation: Cancer patients or those delaying kids can freeze eggs or embryos for later.
No matter the reason, IVF adapts. It’s like a customizable toolkit for building a family.
What Are the Odds? Success Rates Unpacked
Success is the big question, right? The truth is, it depends—mostly on age. Here’s the latest scoop from the CDC’s 2022 data:
- Under 35: About 55% of first cycles lead to a live birth.
- 35-37: Drops to 40%.
- 38-40: Around 26%.
- Over 40: Down to 8%, though donor eggs can bump that up.
These numbers are per cycle, meaning one round of IVF. If you try again, your chances often improve. Clinics tweak things based on what they learn each time.
But here’s something new: a 2023 study from the journal Fertility and Sterility found that women using frozen embryos from a previous cycle had a 5% higher success rate than fresh ones. Why? Frozen embryos let doctors time the transfer perfectly with your body’s cycle. It’s a small edge, but it’s exciting progress.
The Emotional Side of IVF
IVF isn’t just about science—it’s a rollercoaster of feelings. One day you’re hopeful; the next, you’re stressed about shots or waiting for results. Studies show 1 in 3 people going through IVF feel anxious or down at some point. That’s normal—it’s a big deal.
Here’s how to cope:
✔️ Talk It Out: A counselor or support group can lighten the load.
✔️ Lean on Loved Ones: Tell them what you need—space or a hug.
✔️ Take Breaks: Step away between cycles if it’s too much.
❌ Don’t Bottle It Up: Ignoring stress can make it worse.
❌ Don’t Compare: Everyone’s journey is different.
One couple I heard about kept a “hope jar”—every positive step, like a good ultrasound, got a note tossed in. It reminded them to focus on the wins, not just the worries.
What Does IVF Cost—and How Do You Pay for It?
IVF isn’t cheap. In the U.S., one cycle averages $15,000-$20,000, including meds and tests. Insurance coverage varies—19 states mandate some fertility help, but it’s spotty elsewhere.
Here’s a breakdown:
| Expense | Cost Range |
|---|---|
| Meds | $3,000-$5,000 |
| Egg Retrieval | $5,000-$7,000 |
| Lab Work | $3,000-$5,000 |
| Embryo Transfer | $1,500-$3,000 |
Money-Saving Tips:
- Look for clinics with payment plans or discounts for multiple cycles.
- Check grants like Baby Quest or CNY Fertility’s programs.
- Ask about mini-IVF—a lower-dose, cheaper option (around $5,000-$7,000).
A fresh twist: Some employers, like Starbucks and Amazon, now offer IVF benefits. In 2024, 42% of big companies covered it, up from 27% in 2020, per Mercer’s benefits survey. It’s worth asking your HR team.
Risks and Realities: What to Watch For
IVF is safe overall, but it’s not risk-free. Here’s what to know:
- Ovarian Hyperstimulation Syndrome (OHSS): Rare (less than 5% of cases), but meds can overstimulate your ovaries, causing bloating or pain. Severe cases need a doctor ASAP.
- Multiple Births: Twins or triplets happen in 15-20% of IVF pregnancies, raising risks like preterm birth.
- Ectopic Pregnancy: A 2-8% higher chance the embryo implants outside the uterus. It’s treatable but serious.
New research from 2024 in Human Reproduction suggests babies born via IVF have a slightly higher risk of birth defects (4% vs. 3% naturally), but it’s still low. Scientists think it’s tied to infertility itself, not IVF.
Pro Tip: Pick a clinic with a solid track record—check their stats on the SART website (Society for Assisted Reproductive Technology).
IVF Myths Busted
There’s a lot of noise out there about IVF. Let’s clear up a few big ones:
- Myth: IVF babies aren’t “normal.”
Truth: They’re just as healthy as other kids. Louise Brown, now 46, is living proof. - Myth: It’s 100% guaranteed.
Truth: It’s a chance, not a promise—success varies by person. - Myth: It’s only for women.
Truth: Men with low sperm count benefit from ICSI just as much.
Interactive Quiz: Is IVF Right for You?
Take a sec to think about your situation with this quick quiz. Jot down your answers!
- Have you been trying to conceive for over a year (or 6 months if over 35)?
A) Yes B) No - Do you or your partner have a known fertility issue (like blocked tubes or low sperm)?
A) Yes B) No - Are you open to medical help to start a family?
A) Yes B) No
If you’ve got mostly A’s, IVF might be worth exploring with a doctor. Mostly B’s? You might not need it yet—or at all. Either way, it’s your call!
The Future of IVF: What’s Coming?
IVF’s evolving fast. Here are three game-changers not talked about enough:
1. AI-Powered Embryo Selection
Clinics are testing artificial intelligence to pick the best embryos. A 2023 trial in Nature Medicine showed AI boosted success rates by 10% over human selection. It’s like having a super-smart assistant in the lab.
2. Lab-Grown Eggs
Scientists are working on making eggs from skin cells (called in vitro gametogenesis). It’s still experimental, but a 2024 study in mice showed promise. This could help people with no viable eggs—like cancer survivors—have biological kids.
3. At-Home Monitoring
New devices let you track your hormone levels at home during IVF, cutting clinic visits. A small 2025 pilot found 85% of users felt more in control. It’s not widespread yet, but it’s a peek at what’s next.
These advances could make IVF cheaper, easier, and more successful in the next decade.
Real Stories: IVF in Action
Meet Sarah, a 38-year-old teacher from Ohio. After three years of trying, she and her husband found out his sperm count was low. They tried IVF with ICSI in 2023. First cycle? No luck. Second cycle, with a frozen embryo? She’s now 6 months pregnant. “It was tough,” she says, “but seeing that heartbeat made every shot worth it.”
Then there’s James and Michael, a couple from California. Using a donor egg and surrogate, their daughter arrived in 2024 via IVF. “It felt like a miracle,” James says. “The science gave us a family.”
These stories show IVF’s power—and its challenges. It’s not always smooth, but the payoff can be life-changing.
Your IVF Action Plan
Ready to dig deeper? Here’s how to start:
- Research Clinics: Look for ones with high success rates and good reviews.
- Talk to a Specialist: A reproductive endocrinologist can map out your options.
- Check Finances: See what insurance or grants cover—don’t guess.
- Build Support: Line up friends, family, or a therapist for the ride.
Not sure where to begin? Call a local fertility clinic for a free consult—most offer them.
Poll: What’s Your IVF Curiosity?
Weigh in! What part of IVF are you most curious about? Drop your vote in your head (or share with a friend!):
A) How it works
B) Success rates
C) Costs
D) Emotional stuff
Your answer might spark your next step—or just satisfy a hunch.
The Bigger Picture: Why IVF Matters
IVF’s more than a procedure—it’s a bridge to dreams. In 2025, with birth rates dropping (1.6 kids per woman in the U.S., per the CDC), it’s helping people who might’ve given up. It’s also pushing science forward, tackling infertility’s root causes.
But it’s personal too. Maybe you’re reading this because you’re weighing options, or maybe you just want to cheer on a friend. Either way, IVF’s story is about resilience—ours and science’s. It’s not perfect, but it’s a heck of a tool.




